NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Protecting PHI is critical for NEMT providers. Non-Emergency Medical Transportation (NEMT) services handle sensitive patient data like medical records, billing information, and trip details. Mishandling this data can lead to serious legal, financial, and reputational risks. Under HIPAA, fines for violations range from $1,280 to $63,973 per incident, with annual caps of $1,919,173, and intentional misuse can result in $50,000 fines or imprisonment.
To safeguard Protected Health Information (PHI) and comply with HIPAA, NEMT providers must:
- Encrypt and securely store PHI (both in transit and at rest).
- Restrict data access using role-based controls and two-factor authentication.
- Train staff on HIPAA requirements with regular updates and documentation.
- Create a breach response plan to handle incidents and notify affected parties within 60 days.
- Use HIPAA-compliant software for scheduling, billing, and communication.
HIPAA Compliance Checklist: Easy to Follow Guide for 2024
HIPAA Requirements for NEMT Providers
For Non-Emergency Medical Transportation (NEMT) providers, following federal rules for handling patient information isn't just about avoiding fines - it's about creating a reliable and trustworthy service that patients and healthcare partners can depend on.
What Is PHI and Why It Matters
Protected Health Information (PHI) is at the heart of every data interaction in NEMT services. PHI refers to any information that can identify a patient and relates to their health, treatment, or payment for healthcare services. This includes details like patient names, Medicaid IDs, pickup and drop-off locations, medical appointment information, GPS tracking data, trip logs, billing records with insurance details, and even voice recordings from dispatch calls. Since NEMT operations frequently handle such sensitive information, providers are classified as "business associates" under HIPAA. This makes them directly accountable for compliance violations.
Key HIPAA Rules for PHI Security
To manage PHI securely, NEMT providers must adhere to three main HIPAA rules: the Privacy Rule, the Security Rule, and the Breach Notification Rule.
The Privacy Rule lays the groundwork for protecting PHI by specifying who can access patient information and under what conditions. For NEMT providers, this means ensuring employees only access the data necessary for their specific roles.
The Security Rule focuses on electronic PHI (ePHI) and requires safeguards to protect it. This involves encrypting data during transmission and storage, implementing secure user authentication, and maintaining audit trails to track every instance of data access. Providers using digital tools like dispatch systems, mobile apps, or cloud-based platforms must ensure these technologies meet HIPAA standards.
The Breach Notification Rule dictates the steps to take if PHI is compromised. If there’s unauthorized access - whether due to a cyberattack, a lost device, or human error - NEMT providers must notify affected patients within 60 days and report the incident to the Department of Health and Human Services.
On top of these rules, the HITECH Act and Omnibus Rule expanded HIPAA's reach, holding business associates, including NEMT providers, directly responsible for violations. Penalties can be steep, with civil fines ranging from $1,280 to $63,973 per violation, capped at $1,919,173 annually. Intentional violations carry even harsher consequences, including criminal penalties of up to $50,000 and one year in prison.
NEMT providers are also required to sign Business Associate Agreements (BAAs) with the healthcare entities they serve. These contracts clearly define responsibilities for protecting PHI, handling data, and responding to breaches. Without a proper BAA, both the NEMT provider and the healthcare entity could face compliance issues.
Protecting PHI isn’t just a box to check - it’s a responsibility that touches every part of NEMT operations, from dispatching and route planning to billing. Ensuring compliance builds not only legal security but also trust with patients and partners.
PHI Security Checklist: Key Areas to Address
Safeguarding patient information in your NEMT operations demands a structured and thorough approach. Below is a checklist covering the critical security measures necessary to stay HIPAA-compliant and protect sensitive data.
Data Encryption and Secure Storage
Encrypt all PHI both in transit and at rest. Use SSL/TLS for data in motion and AES-256 encryption for stored data. Whether you rely on cloud solutions or physical storage, ensure they meet HIPAA standards. For physical devices like hard drives, USBs, and backup systems, disk encryption is essential to prevent breaches in case of theft or loss.
Secure physical records and IT equipment. Lock filing cabinets, limit access to server rooms, and take steps to keep device screens private in shared spaces.
Maintain encrypted backups in multiple secure locations. Regularly test these backups to ensure quick recovery when needed. Keep detailed documentation of your backup schedules and retention policies to demonstrate compliance during audits. Additionally, implement strict access controls tailored to individual roles to further safeguard PHI.
Setting Up Access Controls
Implement role-based access controls. Limit access to PHI based on job responsibilities. For example, dispatchers may need patient pickup details but not billing information, while administrative staff managing insurance claims shouldn’t access driver GPS data. Use strong password policies, enable two-factor authentication, and set automatic logoff timers (5–15 minutes) to prevent unauthorized access.
Verify identities before granting access. Whether it’s an employee, contractor, or healthcare partner, establish procedures to confirm their identity before they access PHI. Adjust logoff timers based on the sensitivity of the data and the work environment.
Adapt access permissions as roles change. Update access levels when employees are promoted, take on new responsibilities, or go on extended leave. Most importantly, revoke system access immediately when someone leaves your organization to prevent unauthorized remote entry. Pair these measures with comprehensive staff training to strengthen your overall security framework.
Staff Training on PHI Security
Provide detailed HIPAA training tailored to NEMT scenarios. Include real-world examples and conduct quarterly refresher sessions. Update training materials regularly to reflect new regulations, and document participation to ensure compliance. This not only increases individual understanding but also reinforces your organization's commitment to HIPAA standards.
Establish clear reporting procedures for security concerns. Make it simple for employees to report potential breaches by clearly outlining who to contact and what steps to take. Foster a supportive environment where staff feel safe raising concerns without fear of blame or retaliation.
Incident Response and Breach Notification
Create and test an incident response plan. Assign roles, monitor for unauthorized access, and set up automated alerts for suspicious activity. Follow HIPAA’s breach notification requirements by documenting incidents, notifying affected patients within 60 days, and reporting to the Department of Health and Human Services. A well-executed response reduces regulatory penalties and helps maintain trust.
Prepare template notification letters, keep patient contact information current, and designate staff to handle breach communications. After any incident or drill, update your response plan to reflect lessons learned, ensuring continuous improvement in your approach to PHI security.
sbb-itb-cef70f4
Using Technology for PHI Compliance
Today's technology simplifies the process of safeguarding Protected Health Information (PHI). It handles encryption, access controls, and compliance documentation while reducing human error. Below, we’ll explore how HIPAA-compliant software and careful vendor evaluations can strengthen your PHI security strategy.
Using HIPAA-Compliant Software
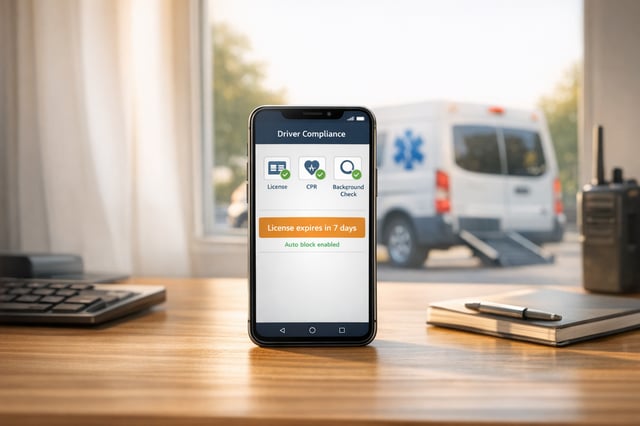
NEMT-specific software automates key compliance tasks like encryption, access logging, and report generation. For example, when dispatchers schedule rides or drivers update trip statuses, the software works behind the scenes to keep PHI secure.
Choose platforms that seamlessly integrate compliance into everyday workflows. The best NEMT software doesn’t just store data securely - it actively enforces compliance. Features like automatic session timeouts, role-specific dashboards, and encrypted communication between drivers and dispatchers ensure PHI remains protected.
Centralized data management reduces risk by consolidating PHI into a single secure system. When all patient data, scheduling, billing, and communication are managed within one HIPAA-compliant platform, you minimize exposure points and streamline compliance oversight.
Modern technologies like Bambi take it a step further by incorporating AI-powered optimization while adhering to strict HIPAA standards. These platforms not only enhance dispatching efficiency and patient care but also maintain robust security, proving that compliance and operational success can go hand in hand.
How to Evaluate Technology Solutions
Once you’ve identified a compliant platform, it’s crucial to assess its security features thoroughly. Here’s how:
Check for encryption of data both in transit and at rest. Ask vendors about their encryption protocols and request documentation of their security certifications to ensure they meet industry standards.
Look for robust user access controls. The software should allow for custom roles, granular permissions, and automatic access logging. Strong security measures like two-factor authentication, strict password policies, and detailed audit trails are essential.
Assess the vendor’s compliance support and documentation. Reliable partners provide Business Associate Agreements (BAAs), regular updates, and tools for compliance reporting. They should also be transparent about their security practices and willing to undergo security assessments if needed.
Evaluate the platform’s incident response capabilities. Test whether the system offers automated alerts for suspicious activity, detailed logging for investigations, and tools to quickly identify affected records in the event of a breach. Some platforms even include pre-built breach notification templates and tools to track reporting deadlines.
Check integration capabilities with existing systems. Software that connects effortlessly with electronic health records (EHRs), billing systems, and healthcare provider networks reduces manual data entry and minimizes security risks from multiple logins.
Research the vendor’s track record and stability. Opt for established companies with proven security histories. Avoid newer platforms that may lack the infrastructure for comprehensive compliance. A vendor’s sudden closure or security breach could leave your organization exposed and non-compliant.
Conclusion: Maintaining PHI Security
Keeping patient information safe is a continuous effort that must adapt to evolving regulations and new security challenges.
The foundation of protecting PHI lies in using secure encryption standards and implementing strict access controls, ensuring that employees access only the data necessary for their specific roles. HIPAA-compliant software can ease this process by automating tasks like encryption, access logging, and audit trails. Many of these platforms, especially those enhanced by AI, also monitor activity and provide breach alerts, reducing the chances of human error or oversight.
However, technology alone isn't enough. Routine audits and ongoing staff training are essential to maintaining compliance. Quarterly compliance audits can uncover vulnerabilities before they escalate into bigger issues. At the same time, mandatory annual HIPAA training ensures that every team member knows their responsibilities when it comes to safeguarding patient data. Tools like secure messaging systems, automated compliance tracking, and centralized documentation management not only enhance security but also improve efficiency. When choosing technology providers, look for those with a solid track record, comprehensive Business Associate Agreements, and strong incident response strategies.
Stay informed by regularly checking government resources and industry updates to ensure your security measures remain up-to-date. Compliance failures can lead to hefty fines and damage your reputation, but by combining well-structured protocols with advanced technology, NEMT providers can effectively protect PHI. This approach not only avoids penalties but also strengthens patient trust - a key ingredient for long-term success in today’s digital healthcare environment.
FAQs
What steps should NEMT providers take to ensure HIPAA compliance and protect PHI?
To meet HIPAA requirements and protect Protected Health Information (PHI), NEMT providers need to prioritize strong security practices. This involves a combination of physical safeguards like locked storage for sensitive records, technical measures such as encryption and two-factor authentication, and comprehensive staff training on HIPAA protocols.
It's crucial for providers to create clear policies for securely handling and transmitting PHI. Employees should be trained on HIPAA requirements within their first week on the job, and regular audits should be conducted to spot and address any security gaps. Additionally, staying up to date with HIPAA regulation changes - like upcoming adjustments to the Security Rule - helps ensure ongoing compliance.
What steps can NEMT providers take to train their staff on securely handling PHI and managing data breaches?
To ensure staff are well-prepared to handle Protected Health Information (PHI) and manage data breaches, NEMT providers should prioritize HIPAA compliance training that's tailored to the specific responsibilities of each role. This training should focus on secure communication practices, proper methods for handling sensitive data, and clear steps for addressing breaches.
Using a mix of interactive workshops, online training modules, and real-world scenarios can make the learning process more engaging and practical. Regular refresher sessions, paired with thorough record-keeping, help keep everyone aligned with compliance standards. Building a workplace culture that emphasizes accountability and vigilance ensures employees can respond swiftly and effectively to any potential data security concerns.
Why should NEMT providers use HIPAA-compliant software to manage PHI, and how can they select the best solution?
Using HIPAA-compliant software is a must for keeping sensitive patient health information (PHI) secure while ensuring your NEMT (Non-Emergency Medical Transportation) services meet strict regulatory standards. These tools protect data with encryption, secure storage, and controlled access, significantly lowering the chances of breaches. Plus, they help build trust with patients by showing a commitment to safeguarding their information. On top of that, many of these solutions simplify compliance tracking, saving you time and helping you steer clear of hefty penalties.
When selecting software, prioritize features like strong security protocols, AI-driven monitoring, and frequent compliance updates. These not only keep you aligned with HIPAA regulations but also enhance your operational efficiency, so you can concentrate on providing top-notch service.