

NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Rural Non-Emergency Medical Transportation (NEMT) providers face two major challenges: dead zones (areas with no cellular coverage) and deadhead miles (empty vehicle trips). These issues drive up costs, reduce efficiency, and make it harder for rural communities to access medical care.
Key Takeaways:
- Dead Zones: Lack of cell coverage disrupts communication and scheduling.
- Solution: Use satellite GPS and tools like Garmin inReach or Starlink for reliable tracking and messaging.
- Deadhead Miles: Empty trips increase fuel costs and waste time.
- Solution: Route optimization software groups rides, reduces inefficiencies, and boosts driver utilization rates.
- Technology Integration: Platforms combining GPS, route planning, and automated billing streamline operations and ensure Medicaid compliance.
By adopting advanced tools and smarter dispatching strategies, rural NEMT providers can reduce costs, improve service reliability, and better serve their communities.
Solving Communication Dead Zones in Rural Areas
What Causes Dead Zones and How They Affect Operations
Dead zones happen when cellular towers are too far apart, and natural barriers - like mountains, valleys, or dense forests - block signal strength. In rural parts of the U.S., where population density is lower, telecom companies tend to prioritize urban areas, leaving many remote regions with spotty or no coverage.
This lack of reliable connectivity can severely disrupt operations. Dispatchers may struggle to send real-time updates or receive confirmations, leading to missed appointments, wasted fuel, and delays in service. As NEMT Cloud Dispatch highlights:
In today's modern world and hustle and bustle, manually operating any business has become almost impossible.
These connectivity challenges call for dependable technology to fill the gaps.
Using Satellite GPS for Reliable Tracking
Satellite GPS offers a dependable tracking solution because it doesn’t rely on cellular networks. This makes it ideal for remote areas. NEMT software leverages satellite GPS to provide live tracking, allowing dispatchers to monitor vehicle status in real time - even when there's no cellular signal. Additionally, Geographic Information Systems (GIS) enhance route planning and fleet management by using precise geographic data, reducing reliance on guesswork.
Telecommunication Tools for Remote Areas
In addition to satellite GPS, specialized telecom devices help address connectivity challenges. Devices like the Garmin inReach Messenger series use the Iridium satellite network for two-way messaging. For instance:
- Garmin inReach Messenger Plus (~$500): Sends photos and voice memos via satellite and can last up to 25 days in low-power mode.
- Garmin inReach Messenger (~$300): A more budget-friendly option for basic messaging needs.
Both models offer "breadcrumb" tracking, enabling dispatchers to follow a vehicle's progress on a web-based map, even in areas without cellular coverage. Other options include:
- SPOT X (~$250): Features a physical keyboard for easier messaging.
- ACR Bivy Stick (~$300): Offers flexible activation plans and lower long-term costs.
For operations requiring full internet access - such as retrieving electronic health records or conducting video consultations - the Starlink Mini provides high-speed satellite internet. This system costs around $499, with monthly plans starting at $50 for 50GB of data. These tools ensure rural NEMT drivers stay connected, even when traditional communication methods fail.
Rural NEMT Solutions (Bambi): Insights from WellTrans' Ray Hagan | NEMT Experts Podcast 58
Cutting Deadhead Miles with Route Optimization
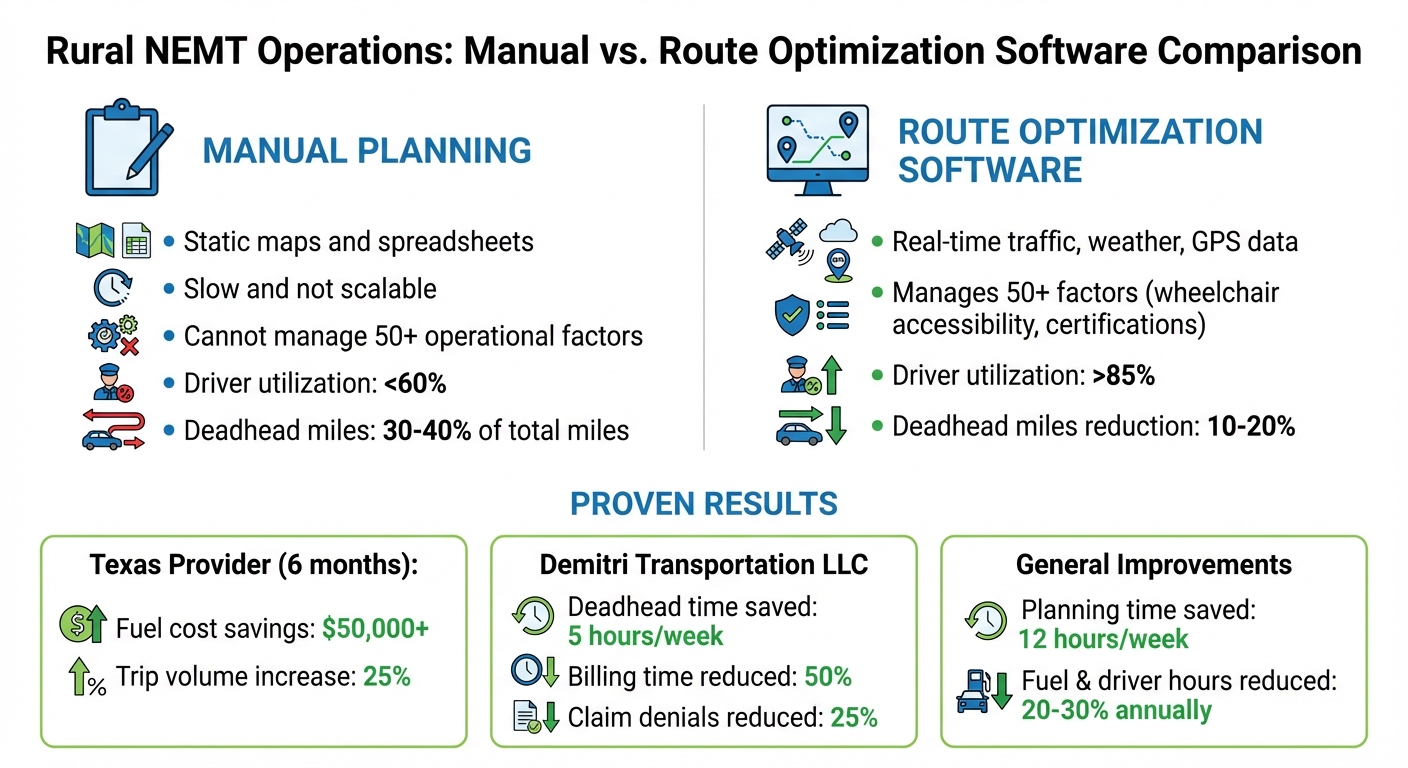
Manual vs Automated NEMT Dispatching: Cost Savings and Efficiency Gains
Why Deadhead Miles Are Higher in Rural Areas
Deadhead miles can seriously impact the profitability of rural NEMT services, accounting for 30–40% of total miles driven. In rural areas, medical facilities are often far apart, and ride requests are less frequent. This means a driver might drop off a passenger 30 miles away and then drive back empty, waiting for the next trip. With fewer patients spread across large areas, it’s nearly impossible to manually coordinate back-to-back rides, leaving vehicles empty for significant portions of their shifts. That’s where route optimization software steps in to address these inefficiencies.
How Route Optimization Software Works
Route optimization software uses advanced algorithms to minimize deadhead miles by evaluating thousands of trip combinations in seconds. For instance, the system can group passengers traveling to similar destinations - like dialysis patients heading to the same clinic - into shared rides, filling up vehicles more efficiently.
AI-powered dispatching also assigns return trips to vehicles already on the road by matching rides based on proximity and availability. The software recalculates routes instantly, avoiding unnecessary empty returns. On top of that, predictive demand forecasting analyzes past trends to predict peak times, enabling providers to position their fleets near high-demand areas. This automated process eliminates the guesswork and inefficiencies of manual scheduling, as explained further below.
Manual Planning vs. Route Optimization Software
Automated routing systems consistently outperform manual scheduling. For example, a mid-sized NEMT provider in Texas cut fuel costs by over $50,000 and increased monthly trip volume by 25% within six months of implementing route optimization software.
Demitri Transportation LLC experienced similar benefits:
"We're saving at least 5 hours a week in deadhead driving time using RouteGenie's dispatching suggestions." – Kelnisha W., Demitri Transportation LLC
This company also reduced the time spent on billing by half and saw a 25% drop in claim denials. In contrast, manual planning - relying on static maps and spreadsheets - is slow and not scalable. Automated systems integrate real-time traffic, weather, and GPS data, while managing over 50 operational factors, such as wheelchair accessibility and driver certifications, that would overwhelm human planners. With automation, driver utilization rates can jump from under 60% to over 85%, and AI-driven routing can cut deadhead miles by 10–20%.
sbb-itb-cef70f4
Technology Tools for Rural NEMT Efficiency
Combining GPS and Route Optimization in One Platform
Modern platforms now combine live GPS tracking with dynamic route optimization, making it easier to adjust for last-minute changes like cancellations or new bookings. This eliminates unnecessary travel and simplifies operations by consolidating these key functions into one system.
These tools also automate trip validation by logging timestamps and location data digitally, ensuring compliance with Medicaid's reimbursement requirements. States such as Texas, New Jersey, and Florida have made electronic GPS validation mandatory for NEMT trip reimbursements. Without these verified logs, providers risk claim rejections at rates between 15–20%, potentially losing up to $50,000 annually.
To address connectivity challenges in rural areas, mobile apps offer offline functionality, allowing drivers to access routes without a signal. Additionally, the software accounts for critical factors like wheelchair accessibility, vehicle capacity, and traffic conditions. These features collectively help rural NEMT providers achieve notable efficiency improvements, as shown in the examples below.
Examples of Rural NEMT Providers Using Technology
By adopting integrated platforms, some providers have cut their planning time by as much as 12 hours per week and reduced fuel and driver hours by 20–30% annually.
Using open data standards like GTFS and TDS further streamlines operations, enabling smooth data sharing across scheduling, dispatch, and billing systems. Open standards offer a cost-effective way for different transportation providers to exchange data seamlessly. On the other hand, proprietary standards often require expensive custom programming and can trap providers into relying on a single vendor.
Conclusion: Improving Rural NEMT Operations
Tackling Dead Zones and Deadhead Miles
To address the unique challenges in rural Non-Emergency Medical Transportation (NEMT), combining satellite GPS tracking, route optimization, and offline telecommunication tools into a single platform is a game-changer. This approach not only bridges connectivity gaps but also helps reduce wasteful deadhead miles.
Collaboration is another key strategy. Shared ride programs, supported through interagency coordination, can significantly improve revenue efficiency. For example, federal NEMT spending through the Department of Health and Human Services hit at least $1.3 billion in fiscal year 2012, making coordinated resource use a financially savvy move.
Another way to streamline operations is by adopting open data standards like GTFS and TDS. These standards prevent vendor lock-in and make it easier to share data across scheduling, dispatch, and billing systems. This flexibility becomes increasingly important as operations expand.
Once these solutions are in place, the next step is to act on them effectively.
Practical Steps for Rural NEMT Providers
Start by assessing your current operations. Track your weekly deadhead miles and identify connectivity gaps to establish a baseline for improvement. This data will guide your next moves.
Then, explore Approved Transportation Management Systems (ATMS) that combine GPS tracking, route optimization, and automated billing into one user-friendly interface. To support these upgrades, consider applying for FTA Section 5310 grants, which can help cover the costs of transit-related IT systems, including scheduling and routing software.
Lastly, connect with state or regional coordination groups to find ride-sharing opportunities with other providers. By investing in advanced technology and fostering collaboration, you can enhance healthcare access for rural communities while boosting your operation's efficiency and profitability.
FAQs
How do GPS systems help NEMT providers improve rural dispatching?
GPS technology brings a lot to the table for rural NEMT providers, offering precise, real-time tracking that helps dispatchers keep tabs on vehicles through an interactive map. With this feature, dispatchers can assign the nearest driver to a new pickup, cutting down on deadhead miles, trimming fuel expenses, and ensuring patients are picked up promptly and efficiently.
Even in areas with spotty cell coverage, GPS systems don’t miss a beat. They rely on satellite communication to keep location data flowing, allowing dispatchers to stay connected with drivers. This ensures accurate ETAs can be shared with patients and caregivers, boosting reliability, reducing missed appointments, and building trust in the service.
When GPS is paired with scheduling software, it unlocks even more possibilities. Providers can analyze trip data to fine-tune routes, group pickups and drop-offs, and cut operational costs further. These tools are game-changers for delivering better service and staying efficient in rural areas.
How does route optimization software benefit NEMT providers in rural areas?
Route optimization software is a game-changer for NEMT providers, streamlining trip planning by automatically determining the most efficient routes. By cutting down on deadhead miles - those empty trips without passengers - it helps save fuel, reduce vehicle wear, and lower overall operating costs. Plus, it keeps drivers on schedule, minimizing missed appointments and improving patient satisfaction.
On top of that, features like real-time tracking and navigation boost safety and dependability. Meanwhile, analytics tools offer valuable insights into trip trends, helping providers refine their operations over time. For many, this technology leads to noticeable cost savings and better on-time performance, making it especially effective in improving services for rural communities.
What are the best ways for rural NEMT providers to reduce deadhead miles?
Rural Non-Emergency Medical Transportation (NEMT) providers can cut down on deadhead miles by incorporating GPS-based tracking and route optimization software. These tools ensure that the nearest available vehicle is assigned to each trip, reducing unnecessary driving and wasted fuel.
On top of that, using predictive analytics to group trips and fine-tune schedules can make operations even more efficient. Thoughtful route planning and trip consolidation not only trim fuel expenses but also save time and improve service quality for patients in rural communities.


