NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
HIPAA compliance is a must for Non-Emergency Medical Transportation (NEMT) providers. Why? Because you handle sensitive patient data daily - like schedules, medical details, and billing info. Without proper safeguards, your organization risks fines up to $50,000 per incident and reputational damage.
Here’s the core issue: access control. It ensures only the right people access the right information. But many NEMT providers fall short, facing problems like shared logins, over-permissioned roles, and missing audit trails. These gaps not only slow operations but also increase the risk of data breaches.
Key fixes include:
- Assigning unique user IDs to track activity.
- Implementing role-based access controls (RBAC) so staff only see what they need.
- Using two-factor authentication and encryption for extra security.
- Running regular audits to catch vulnerabilities early.
- Training employees on HIPAA rules and secure data handling.
The takeaway? Strong access controls protect your patients, avoid hefty fines, and keep your business running smoothly. Start by choosing HIPAA-compliant software, documenting policies, and staying updated on regulations.
Non-Emergency Medical Transportation (NEMT) Coordination Topics #2 of 4 (Mar. 31, 2022)
Common Access Control Problems in NEMT
Many Non-Emergency Medical Transportation (NEMT) providers face challenges with implementing effective access control measures. These issues not only create operational risks but can also lead to costly violations. Recognizing these common problems is a crucial step in building a more secure and compliant operation. Below, we’ll dive into some of the most frequent access control issues, particularly where NEMT providers often fall short of meeting HIPAA standards.
Staff Accessing PHI Without Permission
A common access control failure in NEMT operations occurs when employees access Protected Health Information (PHI) beyond what their job responsibilities require. One key culprit? Shared login credentials. When multiple staff members - like dispatchers, drivers, and administrative employees - use the same username and password, it becomes nearly impossible to track who accessed sensitive data and when.
Another issue is granting excessive access permissions. For instance, drivers may have access to detailed medical histories when all they need are pickup locations and times. Similarly, dispatchers might view sensitive billing information that has no relevance to their role. According to the Department of Health and Human Services, unauthorized access is one of the leading causes of HIPAA breaches across healthcare organizations, including NEMT providers.
This lack of control leads to significant risks. Employees with access to unnecessary information are more likely to inadvertently disclose it. For example, a driver might casually mention a patient’s medical condition during a trip, or administrative staff could discuss private details in an inappropriate setting. Each instance of improper access can result in fines of up to $50,000 per violation, making this a costly oversight for NEMT providers.
Next, let’s explore how poorly implemented role-based permissions contribute to these challenges.
Poor Role-Based Permissions
Role-based access controls (RBAC) are essential for managing who can access specific information, but implementing them effectively is a hurdle for many NEMT providers. Unlike traditional healthcare settings, NEMT operations involve a diverse workforce - dispatchers, drivers, billing staff, and administrative personnel - each requiring different levels of access to patient data.
The problem arises when roles overlap. For example, dispatchers might occasionally handle billing inquiries, or drivers might need to review updated medical equipment requirements for a patient. To prevent workflow disruptions, many providers grant broad access rather than tailoring permissions to specific needs. This approach, however, violates HIPAA’s "minimum necessary" standard, which mandates that employees only access information essential to their job functions.
Poorly designed RBAC systems also lead to inefficiencies. When employees have access to irrelevant data, they waste time navigating through unnecessary information. For instance, a driver might sift through detailed medical records when all they need are basic transport instructions. Over time, these inefficiencies slow down operations and increase the likelihood of mistakes.
Another concern is access creep, which occurs when employees retain permissions they no longer need after changing roles or leaving the organization. Without regular updates to access controls, former employees or staff in new positions could still access sensitive information, creating ongoing compliance risks that are often overlooked.
Missing Audit Trails and Monitoring
The lack of comprehensive audit trails and monitoring systems is another critical issue for NEMT providers. Many operate without proper logging mechanisms, making it impossible to track who accessed patient data, when it happened, or what information was viewed or modified.
This lack of visibility creates blind spots that allow unauthorized access to go unnoticed for extended periods. For instance, a provider might only discover that an employee accessed PHI inappropriately after a patient complaint or during a routine audit. By then, the damage is often done, and the organization may be unable to determine the full extent of the breach.
The consequences don’t stop at compliance violations. Without audit trails, organizations miss warning signs of potential insider threats or system compromises. For example, repeated access to patient records outside an employee’s normal duties could indicate misuse, but without monitoring systems, these patterns remain undetected until a more severe incident occurs.
HIPAA specifically requires detailed audit controls to log and monitor access to electronic PHI. Providers without these systems face significant challenges during compliance audits or breach investigations. The inability to produce detailed access records often results in enforcement actions by the Office for Civil Rights, including hefty fines and mandatory corrective action plans.
This documentation gap becomes especially problematic during incident response. When a breach occurs, providers without audit trails cannot quickly identify the source, scope, or duration of unauthorized access. This delays required breach notifications and increases regulatory penalties, as organizations must assume the worst-case scenario when they lack evidence to prove otherwise. Ultimately, failing to maintain proper monitoring systems creates compliance risks that can jeopardize the long-term viability of NEMT operations.
HIPAA Access Control Requirements for NEMT Providers
HIPAA access control requirements are essential for protecting patient data and ensuring smooth operations for NEMT providers. Here are three key measures every provider should adopt.
Unique User Identification
Every staff member who accesses PHI (Protected Health Information) must have their own unique username or ID. This eliminates shared logins, making it easier to track actions and hold individuals accountable.
For example, when Sarah, a dispatcher, logs into your scheduling system, her unique credentials allow the system to identify her activities. This kind of traceability is invaluable during audits or in the event of a data breach investigation. It also helps monitor productivity and flags unusual behavior.
Most HIPAA-compliant software automatically assigns unique user IDs when creating new accounts. However, it's essential to ensure these IDs remain exclusive throughout an employee's time with the organization and are promptly deactivated when they leave.
To further enhance security, role-based access controls should also be implemented.
Role-Based Access Controls (RBAC)
RBAC ensures employees only access the information necessary for their specific tasks, aligning with HIPAA's "minimum necessary" standard. This approach minimizes the risk of accidental or unauthorized data exposure.
For instance, dispatchers might need access to pickup locations, appointment schedules, and any special transportation needs but don’t require detailed medical histories or billing data. Similarly, drivers should only access basic patient identification and trip details, not full insurance or payment records. For employees with overlapping roles, temporary access permissions can be granted instead of broader, permanent access.
Setting up RBAC involves clearly defining job responsibilities and regularly reviewing access permissions to ensure they align with current roles and organizational changes.
Authentication and Encryption
Strong authentication and encryption are the final layers of defense, building on unique user IDs and RBAC. Implementing two-factor authentication (2FA) alongside robust password policies ensures that only authorized users can access PHI, even if a password is compromised.
Providers should enforce password complexity, require regular updates, and block the reuse of recent passwords. These measures significantly reduce the risk of unauthorized access.
Encryption safeguards patient data both in storage and during transmission. By using industry-standard encryption protocols, intercepted data remains unreadable without the proper decryption keys. Even though most modern HIPAA-compliant platforms handle encryption automatically, it’s crucial to verify that your software encrypts data both "at rest" and "in transit."
For example, a mid-sized NEMT provider in Texas saw unauthorized PHI access incidents drop from seven to zero in just six months after implementing these measures.
sbb-itb-cef70f4
How to Implement Access Control Solutions
Implementing effective access control is about more than just meeting HIPAA requirements - it’s about ensuring your systems, staff, and daily operations work seamlessly together. Here’s how NEMT providers can create a secure and efficient system that protects sensitive information while supporting their workflows.
Using HIPAA-Compliant Software
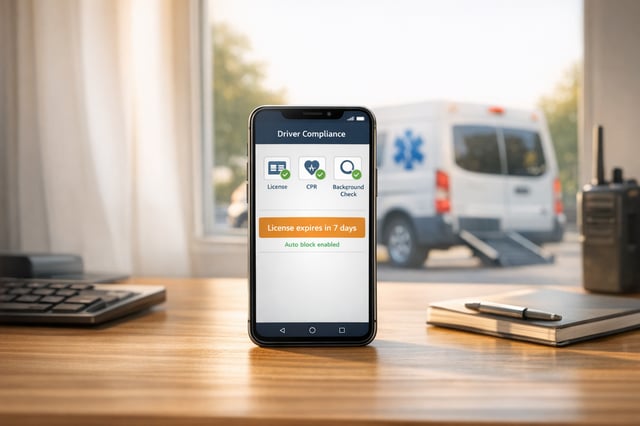
The first step in building a solid access control system is selecting software designed specifically for HIPAA compliance. This means choosing platforms that provide end-to-end encryption, unique user authentication (like usernames, passwords, or biometrics), and role-based access control (RBAC) to limit who can view or modify protected health information (PHI).
Look for software that includes features like audit trails, secure messaging between drivers and dispatchers, and automatic logoff to reduce the risk of unauthorized access. For instance, in 2023, Tobi, a NEMT software provider, introduced advanced user authentication and centralized secure storage. These features helped NEMT providers maintain detailed audit records and streamline compliance documentation, improving their readiness for audits and reducing the chances of unauthorized access to PHI.
When reviewing software options, make sure the platform encrypts data both at rest and in transit. Centralized secure storage is another must-have to ensure sensitive records are properly protected.
Running Regular Security Audits
Security audits are a critical part of maintaining access control systems. These audits help identify weaknesses and ensure your safeguards remain effective over time. Plan for quarterly audits - both internal and third-party - to review your systems, document any findings, and address vulnerabilities as soon as possible.
During these audits, examine access logs to confirm that only authorized users are accessing PHI. Test encryption protocols to ensure they’re functioning correctly, and double-check user permissions, ensuring that employees who have changed roles or left the organization no longer have access to sensitive data.
This proactive approach can prevent small issues from snowballing into major compliance breaches. It’s worth noting that over 60% of healthcare data breaches involve unauthorized access or disclosure, underscoring the importance of regular checks.
Staff Training and Policy Development
Even the best access control systems can fail without proper staff training. NEMT providers should conduct annual HIPAA training for all employees handling PHI. Incorporate hands-on simulation exercises to prepare staff for real-world scenarios and reduce the risk of accidental disclosures.
Training should cover practical topics like secure data handling, recognizing phishing attempts, and using access control systems correctly. Dispatchers need to understand their specific access responsibilities, drivers should know what information they’re allowed to view, and administrative staff must be clear on their role in maintaining security.
Develop clear, written policies that outline access control procedures and staff responsibilities. These policies should be easy to understand and readily available to all employees. Include specific examples, such as steps to take if someone accesses the wrong patient’s information or suspects a security breach.
As cyber threats and regulations continue to evolve, regular refresher training and policy updates are essential. Reinforce best practices with periodic training sessions to ensure everyone stays informed and vigilant.
Staying Compliant and Audit-Ready
Keeping access control systems compliant and prepared for audits requires consistent documentation, careful planning, and staying informed about regulatory updates. For Non-Emergency Medical Transportation (NEMT) providers, this is not a one-time task but an ongoing effort. Success in this area depends on paying close attention to these essential elements and ensuring every control measure is well-documented for potential audits.
Documenting Access Control Measures
To demonstrate HIPAA compliance, it's critical to maintain comprehensive records of access policies, system updates, training sessions, and procedural changes.
Start by creating clear, written security policies that define who has access to specific information and under what conditions. Keep detailed logs of Protected Health Information (PHI) access, including who accessed it and when. Additionally, document risk assessments and any corrective measures taken. Training records are equally important - record dates, attendance, and materials covered during employee training sessions. These details can make a significant difference when auditors review your compliance efforts.
Organized documentation is key. A well-structured storage system allows you to quickly retrieve evidence of compliance, rather than scrambling to locate scattered records. This approach not only saves time but also demonstrates your dedication to safeguarding patient data.
For example, in January 2023, a large hospital network faced a data breach investigation. The organization avoided severe penalties by presenting thorough documentation of their access control measures and incident response. Their audit logs and training records played a pivotal role in convincing the Office for Civil Rights to reduce the fine.
Once your documentation is in place, the next step is to prepare a solid incident response plan.
Incident Response Planning
Even the best access control measures can't fully eliminate the risk of breaches. That's why having a well-documented incident response plan is essential - it can mean the difference between a manageable issue and a major compliance violation.
Your plan should outline steps for containing breaches, mitigating damage, and notifying affected individuals and regulatory authorities as required under HIPAA's Breach Notification Rule. Clearly define roles and responsibilities so that everyone knows what to do in the event of an incident.
When a breach occurs, document every detail: the nature of the incident, the data affected, actions taken to contain the breach, and any required notifications. This documentation not only proves compliance but also helps identify gaps and improve future safeguards.
The financial risks of failing in this area are substantial. In 2022, the average cost of a healthcare data breach reached $10.93 million. Additionally, as of 2023, the Office for Civil Rights has issued over 100 enforcement actions for HIPAA violations, with penalties ranging from $100 to $1.5 million per violation based on severity and negligence.
Staying Updated on HIPAA Regulations
HIPAA regulations and enforcement priorities are constantly evolving, which means compliance is not a static achievement. Regular reviews of access control policies - at least once a year or whenever significant changes occur in technology, regulations, or organizational structure - are essential.
Document any policy updates to ensure they align with the latest HIPAA requirements. This proactive approach allows you to stay ahead of regulatory changes rather than scrambling to adapt after the fact.
The healthcare industry is increasingly moving toward automated audit trails and centralized documentation systems, reflecting the growing importance of continuous compliance efforts. With heightened regulatory scrutiny, many organizations are investing in regular staff training and updating policies to avoid penalties.
HIPAA's Security Rule is intentionally technology-neutral, allowing organizations to adapt their access control measures as new technologies and threats emerge. While this flexibility is beneficial, it also requires staying informed about both technological advancements and regulatory expectations.
To stay current, monitor official HIPAA updates and consider joining professional associations or consulting with compliance experts. These resources can help you navigate complex regulatory landscapes and ensure your access control strategies remain effective and compliant.
Conclusion: Building Better Access Control for NEMT Success
Effective access control isn't just about meeting compliance requirements - it's about creating a secure and sustainable foundation for your NEMT business. Key elements like unique user identification, role-based access controls, authentication protocols, automatic logoff, encryption, and audit controls are essential for achieving and maintaining HIPAA compliance. These measures safeguard both your patients' sensitive information and your organization's reputation.
The stakes are high. With the financial and reputational risks tied to data breaches, implementing strong access control measures isn't optional - it's a necessity. For example, a mid-sized NEMT provider using HIPAA-compliant software with features like role-based access, unique logins, and automatic logoff reported zero PHI breaches over two years. Their success was bolstered by quarterly audits and regular staff training.
Modern technology makes compliance more manageable. Cloud-based, AI-powered NEMT platforms now automate compliance tracking, enhance data security, and reduce administrative workloads. These systems log all user activities, encrypt data in real time, and restrict access based on job roles, making it easier to stay compliant while focusing on your core operations.
To move forward, focus on a few key areas:
- Invest in HIPAA-compliant software: Choose solutions that incorporate essential security features.
- Train your team regularly: Keep staff informed about access control policies and best practices.
- Document everything: Maintain detailed records of access control measures, policy updates, and training sessions to stay prepared for audits.
Above all, foster a security-first mindset across your organization. When every team member understands that access control is about protecting both patients and the business, compliance becomes a shared responsibility rather than a chore. This cultural shift, paired with the right tools and processes, sets the stage for long-term success in a regulated healthcare environment.
FAQs
What happens if NEMT providers don’t follow HIPAA access control requirements?
Failing to establish proper access control measures under HIPAA can spell big trouble for NEMT providers. The risks? Steep financial penalties, potential legal action, and a tarnished reputation. HIPAA violations carry fines that range from $100 to $50,000 per violation, depending on the severity and whether the issue stems from willful neglect.
But the consequences don’t stop there. Non-compliance can erode patient trust and even result in losing contracts with healthcare partners. Limiting access to sensitive patient data to authorized personnel isn’t just about following the law - it’s critical for protecting the integrity and trustworthiness of your NEMT business.
What steps can NEMT providers take to implement role-based access controls and meet HIPAA's 'minimum necessary' standard?
To meet HIPAA's 'minimum necessary' standard, Non-Emergency Medical Transportation (NEMT) providers can use role-based access controls (RBAC). This approach limits access to sensitive information by aligning permissions with employees' specific job roles. In practice, this means staff can only view or use the data they need to perform their tasks, helping to minimize the risk of unauthorized access.
Start by mapping out the roles within your organization - such as drivers, dispatchers, and administrators - and clearly defining the type of information each role requires. Implement secure systems to enforce these permissions and make it a habit to review access logs regularly to monitor compliance. Additionally, invest in training your team on HIPAA regulations and emphasize the importance of protecting patient data to ensure everyone understands their responsibility in maintaining security.
Why should NEMT providers perform regular security audits, and what key areas should they focus on to stay HIPAA compliant?
Regular security audits play a critical role for NEMT providers in maintaining HIPAA compliance and safeguarding sensitive patient information. These audits not only help uncover potential weaknesses but also ensure that access controls are in place and that all systems and processes align with regulatory requirements.
During these audits, it's important to focus on a few key areas:
- Confirming that only authorized personnel have access to patient data.
- Ensuring that patient information is securely stored and transmitted.
- Reviewing and updating policies for addressing breaches or unauthorized access.
By focusing on these aspects, NEMT providers can reduce risks and show their dedication to protecting patient privacy.