

NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Accurate Non-Emergency Medical Transportation (NEMT) billing documentation is essential to ensure claims are processed correctly and payments are received without delays. Every trip must be thoroughly documented to meet federal and state standards, avoid claim denials, and reduce audit risks. Here's what you need to know:
- Key Documentation Requirements: Include patient details (name, Medicaid ID), trip specifics (pickup/drop-off locations, times, mileage), and driver/vehicle information. Use precise formats like 12-hour AM/PM timestamps and MM/DD/YYYY dates.
- State-Specific Rules: Some states require additional forms, prior authorizations, or specific details like trip purpose (e.g., dialysis). Missing these can lead to rejected claims.
- Common Errors: Incomplete logs, missing signatures, incorrect codes, or unverified mileage often result in denials. Up to 50% of claims face initial rejections due to documentation mistakes.
- Prevention Tips: Use GPS-integrated software for tracking, conduct regular audits, and train staff on compliance. Automating processes can reduce errors significantly.
- Technology Benefits: Digital tools simplify record-keeping, ensure compliance, and improve claim accuracy. Features like real-time eligibility checks, EDI integrations, and electronic signatures streamline the process.
Accurate NEMT documentation isn't just about meeting requirements - it's about protecting your revenue and ensuring smooth operations. Missing details or errors can cost you time and money, so focus on thorough record-keeping and leveraging technology to minimize mistakes.
Non-Emergency Medical Transportation (NEMT) Coordination Topics #2 of 4 (Mar. 31, 2022)
Required Elements of NEMT Billing Documentation
When it comes to Non-Emergency Medical Transportation (NEMT) billing, certain documentation is non-negotiable to meet both federal and state compliance standards. At a minimum, you’ll need to include the beneficiary's name and Medicaid ID, pickup and drop-off locations, date and time of service, and the number of loaded miles traveled with the patient in the vehicle. These details are the backbone of any compliant billing claim.
State-specific requirements often add extra layers to this foundation. For instance, you may need to document the trip duration, driver and vehicle details, and the purpose of the trip, such as the type of medical appointment (e.g., dialysis, chemotherapy, or physical therapy). Meeting these standards not only ensures compliance but also makes audits and claims processing much smoother. Let’s break down the key elements.
Trip and Patient Records
Start with the patient’s Medicaid ID and contact details to confirm eligibility for covered services. For pickup and drop-off locations, use exact addresses or GPS coordinates - vague descriptions won’t cut it.
Timestamps should follow a consistent 12-hour AM/PM format. If the trip involves night transportation (starting or ending after 7:00 PM or before 7:00 AM), make sure to document these times in Box 19 of the CMS-1500 form, as this supports proper billing. Clearly state the purpose of the trip, such as whether the patient is heading to dialysis or another medical appointment, to help verify medical necessity during reviews.
For trips requiring prior authorization, include the authorization number in the trip record and in Box 23 of the CMS-1500 form. California regulations, for example, provide exceptions for discharges from acute care to long-term facilities, but you’ll still need to include the referring provider’s NPI in Boxes 17a and 17b. To avoid errors, management should conduct random follow-ups with patients and healthcare facilities to confirm service delivery before claims submission.
Accurate trip records naturally lead to precise mileage documentation, which is another critical element.
Mileage and GPS Data
Mileage documentation must reflect either actual odometer readings from the trip’s start to finish or GPS-tracked route distances, excluding any unnecessary deviations. GPS data is particularly useful, as it provides verifiable proof through coordinates, timestamps, and route maps, which are essential for compliance during audits. States like California require this level of detail for Medi-Cal audits to demonstrate medical necessity and prevent overbilling.
It’s important to record loaded miles separately from deadhead miles (miles traveled without a patient). Automation tools can help identify and minimize deadhead miles, reducing costs while ensuring accurate billing. Always ensure that mileage records align with GPS data and driver logs to avoid audit discrepancies.
Driver and Vehicle Information
Driver details are another crucial component. Include the driver’s full name, valid license number, and NPI (if applicable). Confirm that the driver has a clean record, has passed background checks, and has completed any required drug screenings to meet federal transparency standards. In states like Alaska and Arizona, additional certifications such as CPR and First Aid may also be required, so check your state-specific mandates.
For vehicle documentation, you’ll need details like the make, model, year, license plate number, and VIN, along with proof of ownership that matches your provider entity. Keep current registration, proof of insurance that meets state minimums, and records of regular inspections (e.g., annual safety checks) readily available. For example, a properly documented wheelchair van trip might look like this: "Ford Transit, Plate ABC-1234, inspected 01/15/2025, driver John Doe (License #AZ12345), 15 miles via GPS".
Make sure all vehicles meet ADA standards and have up-to-date safety inspections. Regularly screen both drivers and vehicles against federal exclusion lists to ensure no banned individuals or vehicles are providing services. Keeping accurate and consistent records for drivers and vehicles not only ensures compliance but also protects your claims during audits. Double-check that ownership papers and inspection documents match across all records - any inconsistencies can delay payments or trigger further scrutiny.
HCPCS Codes and Authorization Requirements
After ensuring precise documentation, the next steps - accurate coding and securing prior authorizations - are essential for smooth operations. Correct HCPCS codes and prior authorizations help guarantee timely payments. These codes specify the exact service provided, while prior authorizations confirm that the trip met medical necessity. Mistakes in either area can lead to claim denials, payment delays, or even audit penalties.
HCPCS Codes and Modifiers
HCPCS codes act as the universal billing language for NEMT services. For example, A0130 is the base code for wheelchair van transport, while A0100 applies to ambulatory patients traveling by taxi. For mileage reimbursement, S0215 compensates providers per mile, although some programs exclude payment for the first 20 miles.
Modifiers adjust these base codes to reflect specific trip details, such as trip type, equipment used, or special circumstances. For instance, modifier U1 designates a round trip, whereas modifier HC identifies wheelchair van transport. A standard ambulatory round trip might use A0428 (basic life support mileage) paired with U1, while a wheelchair transport could combine S0215 with HC. In California Medi-Cal, hospital-to-facility transfers often use A0425 (ground mileage) without additional modifiers when authorization requirements are waived.
Mismatched modifiers can result in claim denials that require appeals backed by detailed trip logs. To minimize errors, billing staff should align modifiers with actual trip details, supported by GPS data and driver logs. This accuracy naturally ties into the process of securing prior authorizations.
Prior Authorization Steps
Prior authorization ensures that a transportation service is deemed medically necessary before the trip takes place. Start by verifying patient eligibility through the payer's portal or by phone. Then, submit a detailed request that includes patient demographics, pickup and drop-off addresses, date and time of the trip, estimated mileage, and a medical necessity statement (e.g., "dialysis appointment"). Additionally, a clinician’s prescription or signature and the provider’s NPI are typically required.
Once approved, an authorization number will be issued. Keep all communication records for potential audits. Using electronic systems like EDI 837P transactions can simplify this process, allowing you to attach supporting documents directly to your submission.
In some cases, exceptions exist. For example, California's CCR Title 22, Section 51323(b)(c) exempts NEMT services from acute care hospitals to long-term care facilities from requiring an authorization number, prescription, or clinician signature. While full trip documentation is still necessary, the authorization number in Box 23 can be omitted. Other states have their own rules: Arizona requires a PT-28 packet and AHCCCS enrollment, while New York enforces strict documentation through NYSDOH registration.
To prevent delays, consider conducting random checks with patients and healthcare facilities to confirm that the documented service took place. Automation tools that cross-check HCPCS codes and modifiers against trip data can also reduce errors by up to 50%, helping ensure compliance.
For more expert advice, visit NEMT Entrepreneur (https://nemtrepreneur.com).
sbb-itb-cef70f4
Common Documentation Errors and How to Prevent Them
Common NEMT Billing Documentation Errors and Prevention Strategies
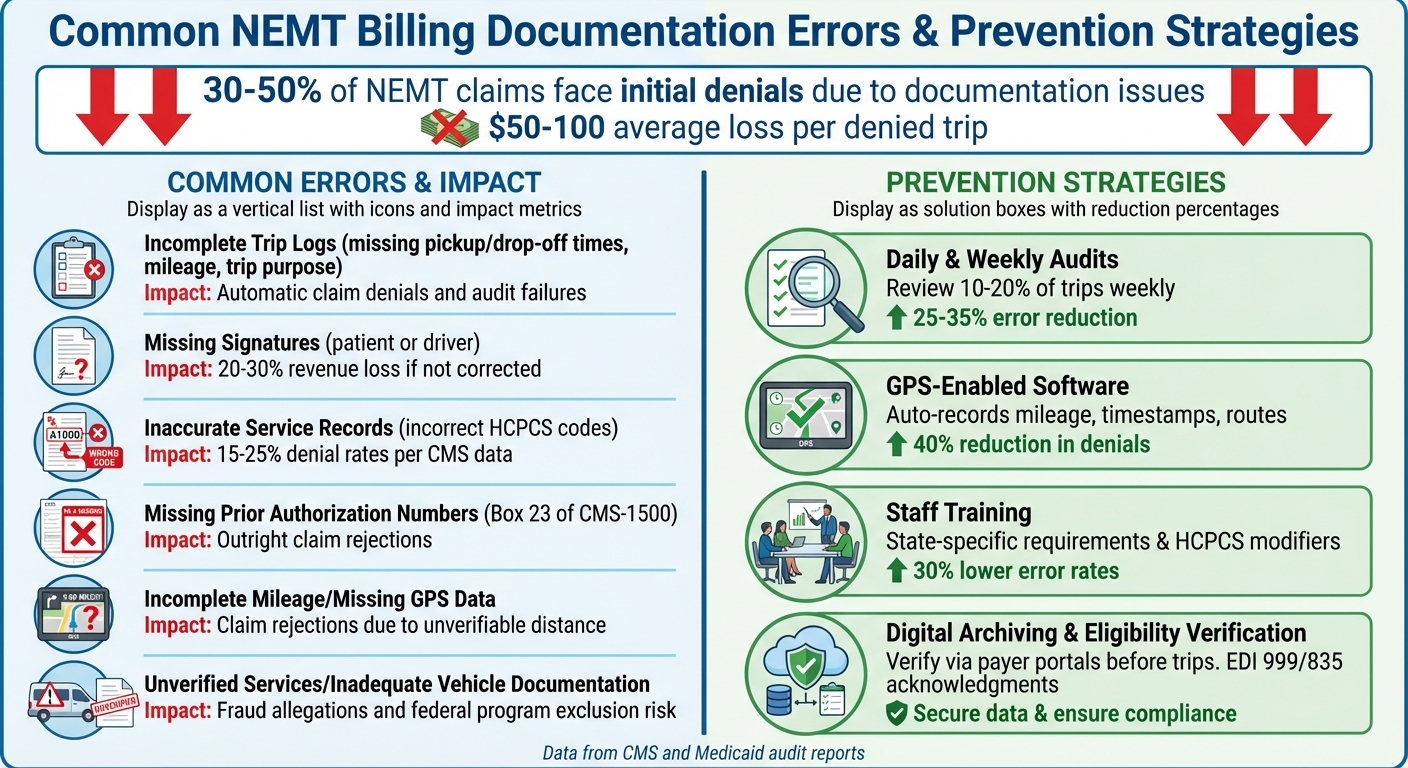
Even with thorough coding and proper authorization processes, documentation mishaps can still throw a wrench into billing operations. Industry statistics reveal that 30–50% of NEMT claims face initial denials due to documentation issues, with Medicaid audits recovering only 60% of denied claims through appeals. These errors come with a hefty price tag - providers lose an average of $50–100 for every denied trip. Spotting these mistakes is the first step toward putting effective prevention strategies in place.
Most Common Errors and Their Impact
Knowing which documentation errors cause the most trouble can help prioritize prevention efforts. Here’s a breakdown of common mistakes and their consequences:
| Common Error | Impact |
|---|---|
| Incomplete trip logs (e.g., missing pickup/drop-off times, mileage, or trip purpose) | Leads to automatic claim denials and audit failures [6, 11] |
| Missing signatures from patients or drivers | Accounts for 20–30% revenue loss if not corrected; causes delays in reimbursements and increases appeal costs [4, 8] |
| Inaccurate service records (e.g., incorrect HCPCS codes for wheelchair trips) | Results in 15–25% denial rates per CMS data and triggers payer audits [7, 8] |
| Missing prior authorization numbers in Box 23 of CMS-1500 | Causes outright claim rejections (except for hospital-to–long-term care transfers) |
| Incomplete mileage or missing GPS data | Leads to claim rejections due to inability to verify medical necessity and distance [3, 8] |
| Unverified services or inadequate vehicle documentation | Raises fraud allegations and risks exclusion from federal programs [3, 6] |
These errors don’t just disrupt cash flow - they also increase compliance risks. For example, missing signatures often result in automatic denials because they fail to confirm trip completion or patient consent [4, 8]. Similarly, incomplete mileage or absent GPS data leads to immediate rejections since payers require this information to verify both medical necessity and reimbursement eligibility [3, 8]. Moreover, under the Social Security Act, Medicaid providers must maintain detailed records - including beneficiary ID, locations, date/time, and miles traveled - and present them upon request.
How to Prevent Documentation Errors
To tackle these common issues, focusing on prevention is key. Here are some strategies that can help minimize errors and ensure smoother operations:
- Daily and Weekly Audits: Conduct daily reviews of trip logs and weekly internal audits on 10–20% of trips. This process helps catch missing fields, verify mileage accuracy, and flag potential issues before claims are submitted. These measures can reduce errors by 25–35%. Assigning a billing manager to oversee this process adds an extra layer of quality control.
- GPS-Enabled Software: Using GPS technology can significantly cut down errors by automatically recording mileage, timestamps, and routes. This tool prevents 40% of denials caused by inaccurate data and supports real-time compliance checks. Billing software analyses suggest that GPS integration alone can reduce errors by up to 40% [5, 8].
- Staff Training: Regular training on state-specific requirements, HCPCS modifiers, and CMS-1500 fields - combined with mock audits and role-playing exercises - can lower error rates by 30% [5, 6]. Randomly calling beneficiaries and appointment sites to verify documented services before billing ensures compliance with program requirements.
- Digital Archiving and Eligibility Verification: Storing trip data digitally makes it easier to handle appeals quickly. Verifying eligibility via payer portals before trips and using software that provides 999/835 EDI acknowledgments to confirm claim receipt and processing status can also help avoid costly mistakes.
Using Technology for NEMT Documentation
Modern technology has become a game-changer in addressing common documentation errors in Non-Emergency Medical Transportation (NEMT) billing. Digital tools not only reduce mistakes but also speed up reimbursements. By automating data capture, validating claims before submission, and maintaining secure audit trails, these platforms ensure compliance with both payer requirements and HIPAA standards. Switching from paper logs to digital systems helps resolve many issues leading to claim denials while also lightening the administrative load. These advancements pave the way for more accurate billing and smoother audits.
Electronic Billing and GPS Integration
GPS technology plays a crucial role in simplifying NEMT billing. It automatically tracks loaded miles, timestamps, and precise routes, eliminating mileage discrepancies and missing data. When integrated with electronic billing systems, GPS data seamlessly feeds into the 837 Professional Transaction format - the standard for electronic claim submissions. This ensures that the billed amounts align perfectly with the services provided.
Real-time eligibility checks further enhance efficiency. Before a trip begins, the software verifies Medicaid coverage and authorization by accessing Medicaid portals, flagging potential issues that could lead to claim denials. Driver mobile apps also contribute by capturing real-time signatures during pickups and drop-offs, helping to avoid incomplete documentation.
Digital Solutions for Audits
Digital tools extend beyond billing, offering robust support during audits. Cloud-based archiving systems make it easy to retrieve records while ensuring security. These systems store patient demographics, Medicaid IDs, and trip details with immutable timestamps, providing a clear audit trail that shows when records were created and accessed. This is especially valuable for compliance reviews and aligns with HIPAA standards for protecting sensitive health information.
Electronic Data Interchange (EDI) further improves transparency by enabling real-time claim tracking. For instance, 999 acknowledgments confirm that payers have received submissions, while 835 remittance notices provide detailed explanations of payment decisions or denials. With GPS logs, timestamps, and electronic signatures readily accessible, appeals processes become more efficient, increasing the chances of recovering revenue. Providers have reported that automated systems can cut denials from documentation errors by up to 50%, thanks to improved GPS accuracy and pre-validation measures.
Conclusion
Accurate billing documentation is the backbone of your NEMT business, ensuring both financial stability and legal compliance. As the saying goes, "If it's not documented, it didn't happen". Recording every trip detail - like member IDs, timestamps, addresses, mileage, medical purpose, signatures, and driver and vehicle information - creates a solid record that protects your revenue and meets state Medicaid and CMS requirements. Every piece of data, from GPS logs to driver signatures, plays a crucial role in maintaining compliance.
Always consult your state Medicaid NEMT manual for specific guidelines. Documentation standards, coding practices, and record retention policies are shaped by payer rules, so aligning your operations, staff training, and automated systems with these requirements can transform documentation into a strength rather than a challenge.
Best Practices Summary
To maintain the integrity of your records, stick to proven best practices. Start by using an end-of-trip checklist to ensure all required elements are captured. Verify that member eligibility matches records, confirm pickup and drop-off times are accurately logged, document addresses linked to the medical purpose, check that mileage aligns with GPS data, and collect all necessary signatures. If a signature cannot be obtained, document the payer-approved exception reason.
Regular audits are key. Review 5–10% of trips each month to ensure entries are complete and accurate. Look for missing or incorrect fields, categorize errors (such as data entry mistakes or authorization issues), and implement corrective actions to address recurring problems. Tracking denial trends and sharing real examples during staff meetings can help emphasize the importance of precise documentation, making accuracy a measurable goal.
For new or expanding providers, the first 90 days are critical. Familiarize yourself with your state’s billing guides, configure your NEMT software to meet payer-specific requirements, train your team on the significance of each data field, and establish a basic quality assurance process from the start. Resources like NEMT Entrepreneur (aka NEMTreprenuer) at nemtrepreneur.com offer templates, workflows, and checklists to help you avoid common pitfalls and create scalable documentation systems. With the right tools and habits, you can minimize denials and focus on growing your business.
FAQs
What are the most common mistakes in NEMT billing documentation, and how can they be avoided?
Mistakes in NEMT billing documentation often crop up in a few key areas: incomplete or incorrect patient information, coding errors, missing required signatures, and inadequate records of the services provided. These missteps can lead to reimbursement delays and even compliance issues.
To minimize these problems, focus on building a well-trained team that understands billing procedures inside and out. Standardized documentation practices are a must, and regular audits can catch errors before they snowball into bigger issues. Additionally, reliable billing software can simplify workflows and boost accuracy. The secret to avoiding billing headaches? Consistency, attention to detail, and a solid process.
How does GPS technology improve the accuracy of NEMT billing documentation?
GPS technology plays a pivotal role in improving the accuracy of NEMT billing by automatically logging essential trip details like start and end times, travel routes, and mileage. This automation ensures accurate and reliable data for billing, significantly reducing the chances of manual mistakes or inconsistencies.
In addition, real-time location tracking helps verify that routes were followed correctly and services were completed as planned - key factors for meeting regulatory and payer standards. This not only simplifies the documentation process but also boosts billing precision while supporting compliance efforts across the board.
What should NEMT providers know about state-specific billing documentation requirements?
State-specific billing documentation requirements for Non-Emergency Medical Transportation (NEMT) providers across the U.S. can differ significantly, but there are a few shared essentials to note. Providers need to adhere to Medicaid and Medicare regulations, maintain precise records of passenger and trip details, apply the correct service codes, and ensure claims are submitted on time.
That said, each state may have its own forms, documentation protocols, and compliance rules. Following these state-specific guidelines is crucial to avoid reimbursement delays or denials. Staying informed about your state’s current requirements is key to keeping your billing process smooth and compliant.


