

NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
EHR interoperability is transforming how Non-Emergency Medical Transportation (NEMT) providers work by connecting patient transportation with healthcare systems.
This integration allows NEMT providers to access real-time patient data - like medical histories, mobility needs, and appointment schedules - directly from hospitals and clinics. By eliminating manual processes like phone calls and paper records, providers can reduce errors, improve scheduling, and ensure patient safety.
Key Highlights:
- Automated Data Sharing: Reduces errors and keeps patient details updated.
- Better Scheduling: Syncs transportation with appointment changes in real time.
- Compliance Made Easier: Simplifies reporting and meets HIPAA standards.
- Improved Patient Outcomes: Ensures timely rides and tailored transportation for medical needs.
Technologies like APIs, FHIR standards, and middleware enable this integration, even with older systems. While challenges like legacy barriers and user adoption exist, careful planning and collaboration with healthcare partners can help overcome them.
How to integrate with EHR systems like EPIC, Cerner | Jeff Fried, Intersystems
Key Benefits of EHR Interoperability for NEMT Providers
EHR interoperability is reshaping how Non-Emergency Medical Transportation (NEMT) providers operate by seamlessly connecting transportation services with healthcare systems. This integration brings improvements that enhance efficiency and elevate the quality of patient care.
Automated Data Sharing
One of the standout advantages of EHR interoperability is the automation of patient data sharing. Instead of relying on manual processes, information flows directly from healthcare systems to transportation platforms. This reduces the risk of errors in data entry and ensures transportation teams have the most up-to-date patient details.
With this automation, staff can shift their focus from tedious tasks like verifying ride details to more impactful roles such as optimizing routes and improving customer service. Real-time updates also mean transportation providers are immediately informed about any changes in a patient’s condition or medical needs. This ensures timely adjustments, prevents delays, and allows teams to prepare appropriately for each trip.
Better Scheduling and Coordination
Accurate and timely information transforms scheduling into a smoother, more adaptive process. When healthcare providers and NEMT services are synchronized, communication gaps that lead to missed or delayed appointments are eliminated. For instance, if a hospital updates an appointment time, interoperable systems automatically adjust transportation schedules and notify everyone involved.
Coordinating multiple appointments becomes easier when NEMT providers can access a patient’s full schedule across different facilities. This allows transportation coordinators to plan efficient routes that save time and reduce costs while improving convenience for patients. Additionally, real-time data on appointment durations and delays helps optimize pickup times, ensuring smoother transitions without unnecessary waiting.
Easier Compliance and Reporting
EHR interoperability doesn’t just boost efficiency - it also simplifies compliance with regulatory requirements. For Medicaid, for example, automated data capture eliminates the need for manual record-keeping, making reporting much easier.
Security is another critical area where interoperability shines. With built-in encryption and audit trails, systems meet HIPAA standards while maintaining data integrity. Complete trip histories simplify quality assurance reviews, while financial reconciliation with healthcare payers becomes more accurate. By including medical codes and patient eligibility details in trip records, providers can reduce claim denials and speed up reimbursement.
Improved Patient Outcomes
Streamlined operations and better coordination ultimately lead to improved patient outcomes. When transportation aligns perfectly with healthcare schedules, patients are more likely to stick to their treatment plans. Timely pickups and drop-offs mean fewer missed appointments, which directly supports better health outcomes.
Patient safety also improves. Transportation teams are informed in advance about specific needs, such as wheelchair accessibility or oxygen requirements, ensuring the right vehicle is assigned. Access to critical medical information - like allergies, medications, or emergency contacts - enables drivers to respond quickly and appropriately in case of an emergency.
Technologies That Enable EHR Interoperability in NEMT
Connecting healthcare systems with Non-Emergency Medical Transportation (NEMT) services requires a blend of technologies that ensure smooth, secure data exchange. These tools reshape how patient information flows, making transportation coordination faster, more precise, and safer.
APIs for Data Exchange
Application Programming Interfaces (APIs) serve as the bridges between different software systems, allowing them to share data in real time. For NEMT, APIs enable transportation platforms to access patient details from hospital systems, get updates about appointments, and send ride confirmations back to healthcare providers.
APIs operate using a RESTful architecture, which transmits critical details like patient demographics, pickup addresses, medical needs, and appointment times instantly. This eliminates the need for outdated methods like phone calls or faxes that can lead to errors or delays.
Security is a top priority, with OAuth 2.0 authentication and SSL encryption safeguarding sensitive patient data during transmission. These features ensure compliance with HIPAA regulations while keeping information secure. Additionally, APIs maintain logs of all exchanges to meet compliance requirements.
What makes APIs truly powerful is their bidirectional communication capability. NEMT systems can not only receive ride requests but also send updates back to healthcare providers. For instance, if traffic delays a patient, the healthcare facility is notified automatically, allowing them to adjust schedules as needed. APIs also pave the way for adopting standardized frameworks like FHIR.
FHIR Standards for Interoperability
Building on API technology, Fast Healthcare Interoperability Resources (FHIR) sets a standardized framework for healthcare data exchange across systems. Developed by Health Level Seven International (HL7), FHIR ensures that various healthcare systems can process and understand data in the same format.
FHIR organizes information into specific resources - such as Patient, Appointment, and Location - that can be easily shared. For NEMT providers, this means receiving patient data in a consistent format, no matter which hospital or clinic initiated the request.
In the U.S., the Core Implementation Guide for FHIR establishes compatibility across healthcare systems nationwide. This is especially helpful for NEMT providers working with multiple facilities, as it eliminates the need for customizations for each partner’s data format.
FHIR’s modular design allows transportation platforms to pull only the data they need, such as pickup addresses, destinations, mobility requirements, and emergency contacts. This targeted approach reduces bandwidth usage and enhances system efficiency while also limiting unnecessary exposure of patient data.
Another advantage of FHIR is its support for subscriptions. NEMT systems can receive automatic updates when patient information changes. For example, if an appointment is rescheduled or mobility needs are updated, the system is notified immediately, improving scheduling accuracy and reducing errors.
Integration with Legacy Systems
Many healthcare facilities still rely on older EHR systems that use proprietary formats or outdated protocols, which can’t easily connect with modern NEMT platforms. This is where middleware comes in - it acts as a translator, converting data from legacy formats like HL7 v2.x into FHIR resources. This allows older systems to participate in modern, interoperable networks without requiring major overhauls.
For legacy systems that can’t support APIs, database-level integration offers another solution. By connecting directly to legacy databases, integration platforms can extract patient and appointment data through scheduled updates. While not as instantaneous as APIs, this method ensures transportation data remains relatively current throughout the day.
Hybrid architectures provide a flexible solution for healthcare organizations transitioning to modern systems. They allow critical patient data to flow through FHIR APIs while legacy systems continue handling other functions. This phased approach minimizes costs and disruption during the upgrade process.
Additionally, some integration tools offer web-based portals for facilities that can’t automate data exchange yet. These portals allow staff to manually input transportation requests while maintaining standardized data formats. This ensures consistency and accuracy even for facilities that haven’t fully upgraded their technology.
sbb-itb-cef70f4
How to Implement EHR Interoperability in NEMT Operations
Integrating EHR interoperability into Non-Emergency Medical Transportation (NEMT) operations requires a well-thought-out plan, collaborative efforts, and constant fine-tuning. By aligning technology with healthcare providers' needs, you can ensure smoother data exchange and better service delivery.
Evaluate Current Systems
Start by analyzing your current systems and workflows. This includes documenting your hardware, software, and existing processes. Such an assessment helps pinpoint inefficiencies that interoperability can resolve.
Pay particular attention to how your NEMT software interacts with EHR and scheduling systems. Many providers find that outdated APIs or incompatible data formats create unnecessary barriers. To address this, examine your software’s Application Programming Interfaces (APIs) and data standards. If your system doesn’t support modern protocols like FHIR or HL7, you may need to upgrade or replace it.
Security is another critical area. With healthcare data breaches affecting over 250 million individuals in 2024 - a staggering jump from 50 million in 2022 - ensuring compliance with HIPAA standards is non-negotiable. Verify that all components of your system, from mobile apps to cloud infrastructure, are designed to safeguard sensitive data.
Finally, consider factors like transaction volumes, partner system capabilities, and your organization’s growth plans. These insights will guide your next steps.
Choose Interoperable Solutions
Once you’ve assessed your current setup, focus on selecting the right platform. Prioritize solutions that support FHIR standards and advanced APIs, as these are increasingly central to healthcare data exchange.
Security should be a top priority. Opt for platforms built with HIPAA-first principles, featuring encryption, role-based access controls, and multifactor authentication. With fines for HIPAA violations reaching up to $50,000 per incident, compliance protects both your patients and your business.
Look for platforms that streamline processes through FHIR APIs, allowing seamless integration of patient demographics, appointment details, and mobility needs from healthcare partners. Additionally, platforms with continuous monitoring and incident response tools - such as intrusion detection and automated alerts - are essential for addressing today’s cybersecurity challenges.
"NEMT is no longer just about vans and call centers; it is becoming a digital-first healthcare service." - Mindbowser
With the right technology in place, the focus shifts to building strong data-sharing relationships.
Establish Data-Sharing Partnerships
Technology alone isn’t enough - successful interoperability hinges on collaboration with healthcare providers. Start by identifying your most frequent partners and working with them to establish standardized workflows for data sharing.
Define protocols for what data will be shared, when, and how updates will be communicated. Many NEMT providers begin with one or two key partners to fine-tune their systems before scaling up.
Using standardized terminology and coding systems like SNOMED CT, LOINC, and ICD-10 ensures consistency and reduces errors in patient data exchange. Work closely with partners to align on these standards.
Address compliance early by setting up Business Associate Agreements (BAAs). These agreements clearly outline responsibilities for data protection, forming the backbone of secure, compliant partnerships.
Consider the specific timing and volume needs of each partner. For instance, some facilities may require real-time updates for urgent transport, while others can work with batch processing for routine appointments. Tailoring your approach to these preferences ensures smoother operations.
Train Staff and Monitor Results
After setting up systems and partnerships, success depends on proper training and ongoing monitoring. Without these, even the most advanced solutions can fall short.
Develop training programs that cover both the technical aspects of the new systems and the compliance requirements for handling sensitive data. Focus on how interoperability changes daily workflows, such as automating data sharing for ride scheduling and healthcare communication. Hands-on practice with real-world scenarios often helps staff adapt faster.
Track the success of your implementation through key performance indicators (KPIs). Metrics like ride completion rates, appointment accuracy, data transmission errors, and compliance audits can highlight areas for improvement and validate your investment in interoperability.
Security monitoring should also be a continuous effort. Implement tools that track data access and flag unusual activity. Regular security audits ensure your systems remain HIPAA-compliant over time.
Finally, plan for ongoing improvements. Use staff feedback and performance data to refine your processes. Regular reviews with healthcare partners can uncover new opportunities to improve data sharing and patient care coordination.
Statistics underline the importance of getting this right: while 84% of hospitals share healthcare data with external providers, only 44% of care providers feel their EHR systems integrate effectively with others. This gap highlights the need for a thoughtful and thorough approach to interoperability.
Common Challenges in EHR Interoperability
While the advantages of interoperability are clear, implementing it is no walk in the park. For NEMT providers, the road to integrating EHR systems is often riddled with hurdles that can derail even the most carefully crafted plans. Anticipating these challenges can help providers develop strategies to sidestep costly missteps and ensure smoother implementation.
Managing Legacy System Barriers
A major obstacle stems from legacy systems that many NEMT providers still rely on - systems that were never designed to handle modern data-sharing requirements. These older platforms often use proprietary formats and lack the APIs needed for seamless integration. The solution? Middleware. Cloud-based middleware, in particular, can bridge the gap by translating data between outdated and modern systems.
Instead of overhauling everything at once, providers can start small. Upgrading critical components like patient scheduling systems or dispatch software first allows for phased modernization. This gradual approach not only spreads costs over time but also gives staff the chance to adjust to changes without feeling overwhelmed. Partnering with integration specialists can further minimize disruption and ensure a smoother transition.
Ensuring Data Security and HIPAA Compliance
Data security is another significant hurdle. Every time data is exchanged, a new vulnerability arises, and in healthcare, breaches can have severe consequences - not just for patient privacy but also for the provider’s reputation and operations.
To mitigate risks, start with end-to-end encryption for both data in transit and at rest. Standards like AES-256 offer strong protection, but proper implementation requires careful management of encryption keys and access controls. Multi-factor authentication and role-based access controls are also critical. These measures ensure staff members only access the information they need for their specific roles, reducing unnecessary exposure.
Audit trails are another must-have. By tracking all data access and modifications, these logs serve multiple purposes: they help pinpoint security incidents, demonstrate compliance during audits, and hold staff accountable for how data is handled. Automated systems that monitor for unusual access patterns or potential breaches in real time add an extra layer of protection.
Regular security assessments and penetration testing can uncover vulnerabilities before they’re exploited. Many providers work with healthcare cybersecurity firms that specialize in addressing NEMT-specific risks and compliance needs. Beyond meeting regulatory requirements, robust security measures build trust with patients and partners, which is crucial for long-term success.
Driving User Adoption
Even the best technology can fail if users resist it. Staff members often worry that new systems will complicate their workflows or add unnecessary stress. Overcoming this resistance requires thoughtful planning and communication.
Training is key. Show staff how interoperability simplifies their daily tasks - like reducing manual data entry and the need for phone calls - by automating data sharing. Hands-on practice sessions and involving key team members early in the process can make a big difference. Identifying "super users" who can champion the system and assist their colleagues is another effective strategy.
Getting buy-in from healthcare partners can also be tricky. Some facilities may hesitate to share data or adapt their workflows. Building trust with these partners takes time and a clear demonstration of mutual benefits. Start with tech-savvy partners who are open to innovation, and use their success stories to encourage others to join.
Continuous feedback is essential. Regular check-ins with staff can uncover hidden training needs, workflow issues, or technical glitches. Addressing these problems early prevents them from escalating. Tracking progress with specific metrics - like the percentage of rides scheduled through automated systems or fewer data entry errors - provides tangible proof of success and justifies ongoing investment in interoperability efforts.
Tackling these challenges head-on is critical for integrating EHR interoperability into NEMT operations effectively. With careful planning and a focus on collaboration, providers can unlock the full potential of these systems.
Conclusion: The Impact of EHR Interoperability on NEMT
EHR interoperability is reshaping the way Non-Emergency Medical Transportation (NEMT) providers operate by bridging the gap between transportation and healthcare. This integration supports the shift toward value-based care models in the U.S. healthcare system. By adopting interoperable technologies, NEMT providers can improve both operational efficiency and patient outcomes, positioning themselves as essential players in this evolving landscape.
When NEMT providers integrate with Electronic Health Records (EHR), they unlock benefits like better care coordination and streamlined regulatory reporting. Access to patient medical histories, seamless collaboration with healthcare facilities, and automated compliance reporting transform NEMT into a vital part of coordinated care. This aligns with the Centers for Medicare & Medicaid Services' vision, where every step in a patient’s healthcare journey contributes to improved outcomes.
Key Takeaways
EHR interoperability is revolutionizing NEMT operations in several ways:
- Automated data sharing reduces scheduling errors and simplifies workflows.
- Access to patient data enhances safety while cutting operational costs.
- Advanced interoperability systems improve compliance and support better health outcomes.
The technology behind this shift - such as FHIR standards and modern APIs - empowers NEMT providers to scale their operations while focusing on what truly matters: delivering safe, reliable transportation that contributes to better health.
While challenges like legacy systems and user adoption remain, these hurdles can be addressed with thoughtful planning and phased implementation. Providers who take steps now to embrace interoperability will gain a competitive edge as these systems become the industry norm.
Explore More with Bambi
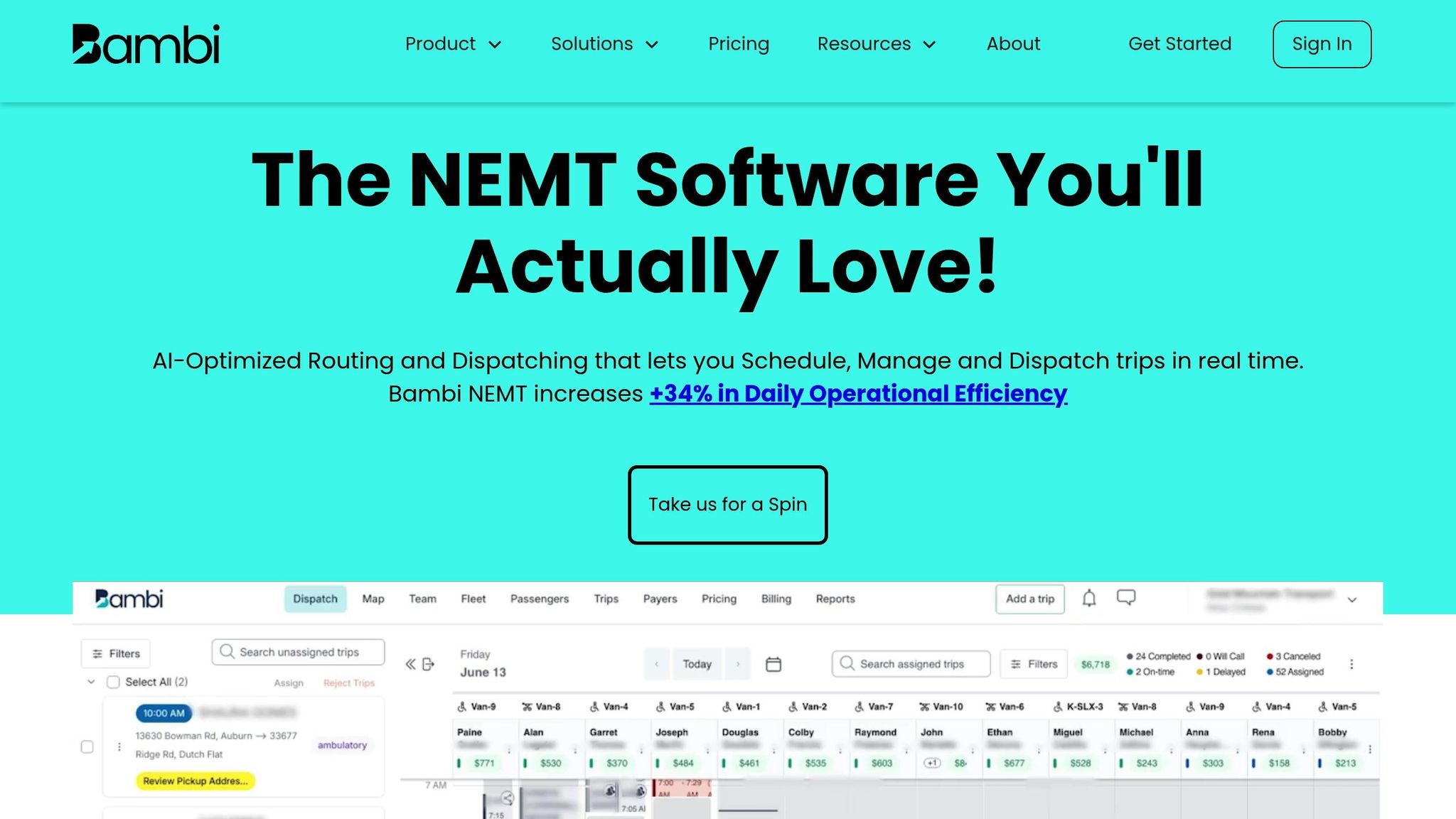
Looking for actionable strategies to make these changes? Visit the Bambi NEMT blog for practical insights on integrating interoperability, leveraging AI-powered tools, optimizing dispatch systems, and ensuring compliance.
Whether you're starting to explore interoperability or refining your current systems, the blog offers valuable resources, including HIPAA compliance guides, success stories, and step-by-step strategies to help you navigate technological and regulatory shifts. Stay informed and ahead of the curve with the tools and knowledge to make smarter decisions for your NEMT operations.
FAQs
How does EHR interoperability improve NEMT scheduling and coordination?
EHR interoperability plays a key role in improving Non-Emergency Medical Transportation (NEMT) scheduling and coordination. By allowing real-time electronic sharing of patient information between healthcare providers and transportation services, it eliminates the need for repetitive manual data entry and reduces the risk of errors. This ensures that transportation planning is based on the most current and accurate medical details, enhancing both safety and reliability.
With streamlined referrals and automated scheduling, interoperability cuts down on administrative tasks, helping to lower costs and boost efficiency. This smooth exchange of information enables NEMT providers to coordinate rides more effectively, resulting in quicker response times and better care for patients.
How do technologies like APIs and FHIR standards support seamless data sharing between NEMT providers and healthcare systems?
Technologies such as APIs and FHIR (Fast Healthcare Interoperability Resources) are essential for facilitating seamless data exchange between NEMT providers and healthcare systems. FHIR leverages modern web technologies like RESTful APIs, JSON, and XML to create a standardized framework for sharing healthcare data. This approach enables secure, real-time integration with electronic health records (EHRs).
When NEMT providers adopt these tools, they can enhance communication, coordinate more effectively with healthcare facilities, and maintain accurate data. This kind of interoperability minimizes errors, improves patient care, and boosts the overall efficiency of NEMT operations.
How can NEMT providers address challenges with outdated systems to successfully implement EHR interoperability?
To address the challenges posed by outdated systems and achieve seamless EHR interoperability, NEMT providers should begin by thoroughly assessing their current technology to pinpoint any weaknesses or risks. This evaluation lays the groundwork for crafting a clear, step-by-step plan to modernize operations without disruption.
Key steps in this process include implementing standardized data exchange protocols, ensuring a careful and secure migration of existing data, and offering thorough training for staff so they’re ready to navigate the updated system effectively. These measures not only bring your technology up to speed but also improve communication with healthcare providers, simplify scheduling processes, and enhance how patient care is coordinated. Prioritizing interoperability allows NEMT providers to work more efficiently and deliver higher-quality service to patients.

