

NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Managing credentials for a Non-Emergency Medical Transportation (NEMT) business can be overwhelming. Driver licenses, vehicle inspections, insurance certificates, and drug test records must be current to meet federal regulations and broker requirements like ModivCare. A single lapse can lead to denied claims, audit failures, or contract termination. Thankfully, automated tools now simplify this process, cutting onboarding time, verifying licenses quickly, and ensuring compliance with real-time monitoring.
Here are the top credential verification tools for NEMT providers:
- VectorCare: Centralizes vendor credentials, automates expiration reminders, and integrates with major EHR systems.
- MedTrainer: Automates license checks, offers managed services, and monitors federal exclusion databases.
- CredentialStream: Links to over 1,000 primary sources, provides real-time verification, and generates NCQA-compliant reports.
- symplr Provider: Tracks credentials across federal databases and offers cloud-based solutions for large networks.
- Verisys: Features the FACIS® database for thorough checks and real-time monitoring of sanctions and exclusions.
- Modio Health: Consolidates credential data into a single profile and tracks compliance with automated alerts.
- Medallion: Uses AI to streamline credentialing, saving time and reducing errors.
- CredentialingSpectrum: Affordable, with real-time checks and integration with CAQH ProView.
- MediRoutes Pro: Tailored for NEMT, manages driver and vehicle credentials while integrating with brokers.
- Bambi NEMT Software: Automates scheduling, routing, and credential-based trip assignments.
These tools improve compliance, reduce administrative workload, and protect your revenue cycle. Whether you're a small provider or managing a large fleet, choosing the right platform ensures your business stays audit-ready and efficient.
Best-In-Class Healthcare Credentialing Software
1. VectorCare
VectorCare takes a unique approach by offering a brokerless system that directly connects healthcare facilities with NEMT (Non-Emergency Medical Transportation) providers. It also handles all credential verification through its Trust module, ensuring a seamless process for healthcare organizations. The platform is free for hospitals and healthcare facilities, making it an accessible option for these organizations. For instance, Kaiser Permanente, one of California's largest payer-providers, relies on VectorCare to schedule thousands of patient transports daily. This system saves case managers countless hours each year by automating workflows and utilizing a network of credentialed vendors [13,14].
Primary Source Verification
VectorCare's Trust module centralizes vendor credentials - like driver licenses, vehicle inspection reports, and insurance certificates - into one secure location. This simplifies the often-tedious process of collecting and verifying credentials. The platform handles about 3.7 transports per minute, allowing hospitals to book services in under three minutes [14,13]. Onboarding workflows ensure vendors meet compliance standards from the start, and a free iOS app allows drivers to easily upload identification and licenses while on the move [12,15].
"VectorCare Trust simplifies credential management and policy enforcement, building a reliable network of qualified vendors while maintaining compliance and operational efficiency." – VectorCare
By streamlining credential verification, the platform lays a strong foundation for effective compliance monitoring.
Compliance Monitoring Features
To keep services running smoothly, VectorCare automatically tracks credential expiration dates and sends reminders at multiple intervals - 60, 30, 14, 7, and 0 days before expiration. Visual tools provide an at-a-glance view of certifications, showing which are active, nearing expiration, or expired. The VectorCare Hub also generates reports that flag potential issues like duplicate charges, mileage padding, and pricing anomalies, which is particularly important given the $16 billion in fraud-related Medicare Advantage mispayments. Additionally, real-time tracking of pickups and drop-offs ensures that services are completed as claimed.
Broker Integration
By eliminating traditional brokers, VectorCare directly connects healthcare facilities with more than 2,500 pre-credentialed vendors. In November 2025, the platform introduced a SMART on FHIR app that integrates with major EHR systems like Epic, Cerner, and Allscripts, enabling users to manage transportation and credentialing directly within their existing workflows [12,14]. Through the Trust module, service providers maintain a single set of digital credentials that can be instantly shared with multiple healthcare organizations, replacing outdated manual processes like faxing and phone calls.
2. MedTrainer
MedTrainer offers an automated, secure solution for managing NEMT credentialing tasks, building on the advanced features seen in platforms like VectorCare. By leveraging a secure API, it automates license checks and integrates seamlessly with CAQH. This allows the platform to verify all types of licenses across all 50 states, instantly pulling license data into the system. As a result, the need for manual tracking of licenses, certifications, and insurance documents is eliminated.
Primary Source Verification
MedTrainer simplifies the credentialing process by automating key verifications. It conducts National Practitioner Data Bank (NPDB) queries and handles checks for DEA, NPI, and board certifications. Each verification is meticulously logged - recording the name, date, time, and source - to create audit-ready documentation. For organizations seeking additional support, MedTrainer offers managed verification services, where specialists oversee the entire process of document collection and verification. According to MedTrainer, 93% of customers find that primary source verifications and exclusions are completed faster, and 95% report quicker payer enrollments.
"Using MedTrainer helps us focus on other aspects of our clinic by cutting down on time needed for our credentialing." – Dana Eberhard, Credentialing/Billing Specialist, FASA Family Wellness, PLLC
Compliance Monitoring Features
To maintain compliance, MedTrainer continuously monitors federal and state exclusion databases, including OIG and SAM, ensuring that neither drivers nor staff are barred from participating in healthcare programs. Automated reminders notify users of expiring licenses and upcoming renewals, reducing the risk of compliance issues that could lead to denied claims. Real-time dashboards provide a clear view of credential gaps, enabling organizations to address potential problems before they escalate. On average, this system saves users 3 weeks per year on credentialing tasks.
"Exclusion checks were such a weight lifted off of my shoulders. We have a huge organization, 300 plus employees and manual exclusion checks were very time-consuming. MedTrainer is the perfect solution!" – Kristina Didonato, Chief Compliance Officer, Community Urgent Care PC
Pricing and Affordability
MedTrainer adopts a "pay for what you need" pricing model, which scales to fit the needs of NEMT providers. For those opting for managed credentialing services, the platform offers one fixed price per provider, covering all verification tasks, document handling, and payer follow-ups. Organizations utilizing these managed services report saving an average of 50% on credentialing expenses compared to managing the process internally. It’s no surprise that MedTrainer is ranked #1 in Healthcare Compliance Software by G2 users. Up next, we’ll look at another leading tool for NEMT credential verification.
3. CredentialStream
CredentialStream, developed by HealthStream, simplifies credential management with automated primary source verification. By connecting to over 1,000 primary sites, it ensures credentials like licenses, board certifications, sanctions, and exclusions are verified in real time, reducing errors and delays. Its OneClick CVO integration allows direct submission of provider records to an NCQA-certified organization without leaving the software, making the process seamless.
Primary Source Verification
CredentialStream handles a wide range of credential verifications, from driver's licenses to board certifications, by directly linking to state licensing boards and federal databases. It centralizes credential data, eliminating departmental silos and ensuring a unified approach. The platform also features a library of 7,000 pre-populated enrollment forms, which are regularly updated, speeding up onboarding processes compared to manual methods. With HealthStream CVO’s expertise in credentialing since 1998, the system benefits from decades of fine-tuned workflows.
"CredentialStream includes integrated tools for real-time, automated primary source verification across a wide range of credentials, including licenses, board certifications, sanctions, and exclusions." - HealthStream
Compliance Monitoring Features
CredentialStream actively monitors federal and state exclusion databases, sending automated alerts well before credential expirations to help avoid disruptions. The platform is HITRUST r2 certified, ensuring top-tier security for provider data. For NEMT providers with delegated payer agreements, it generates detailed reports that meet NCQA, URAC, and CMS compliance requirements.
Pricing and Affordability
CredentialStream offers a tailored solution called "CredentialStream for Groups", designed for small to mid-size organizations. This version skips the more complex features aimed at large acute-care hospitals, making it a practical choice for NEMT businesses. Additionally, using the integrated CVO service can cut costs by reducing the need for individual subscriptions to various industry databases. The platform has earned a 4.5-star rating on SourceForge from 161 users, with reviews highlighting the responsive support team and its cost-effectiveness.
Next, we’ll explore how symplr Provider approaches credential management.
4. symplr Provider
symplr Provider streamlines credential verification for NEMT providers, offering a platform that simplifies the process with automated primary source verification. By directly connecting to state licensing boards and federal agencies, it ensures accuracy and reliability. The platform holds NCQA certification across all 11 verification areas, covering license verification, DEA registration, and education credentials. For providers managing large, distributed driver networks, its cloud-based system enables remote document sharing and online task completion.
Primary Source Verification
Instead of relying on self-reported data, symplr Provider pulls information directly from issuing organizations. For example, in 2024, Hennepin Health in Minneapolis used the platform to credential 60% more providers - jumping from 3,000 to 5,000 - while completing the process 30% faster without increasing staff. Nils Lindahl, Provider Data Steward at Hennepin Health, highlighted the impact:
"Thanks to symplr Payer, we can credential 60% more providers (5,000 up from 3,000) 30% more quickly with the same staff because symplr Payer automates the primary source verification."
The platform processes over 7 million applications annually, and users typically experience a 30% reduction in the time spent on primary source verification tasks. This level of automation supports efficient compliance management.
Compliance Monitoring Features
symplr continuously tracks federal databases like OIG, LEIE, SAM, and the National Practitioner Data Bank to flag sanctions in real time. Automated alerts notify users before driver licenses or certifications expire, helping organizations maintain compliance. The platform also generates audit-ready reports instantly, simplifying state and federal reviews. Backed by HITRUST certification and SOC 2 Type II compliance, symplr ensures strong data security.
Pricing and Affordability
symplr offers custom pricing based on an organization’s specific needs and volume. According to Jim Mihnovich, CFO of Complete Health, their investment in symplr "paid for itself in weeks", allowing immediate cost savings to be redirected to other priorities. By reducing the need for additional staff and improving efficiency, organizations quickly see a return on their investment. In the 2024 Black Book user survey, symplr ranked #1 for Provider Data Management and Credentialing Software, earning 13 out of 18 top scores among 44 competitors.
Next, we’ll take a closer look at Verisys and its approach to credential verification.
5. Verisys
Verisys is known for its impressive 99.9% verification accuracy rate and access to over 5,000 primary sources, including state licensing boards, the Office of Inspector General (OIG), and DEA registrations. By leveraging advanced automation, the platform verifies professional licenses and other critical datasets directly from primary sources, eliminating the need to rely on self-reported information. For Non-Emergency Medical Transportation (NEMT) providers, this means thorough checks not only on medical credentials but also on driver-specific requirements like motor vehicle records and criminal background checks.
Primary Source Verification
At the heart of Verisys' capabilities is its proprietary FACIS® (Fraud and Abuse Control Information System) database. This resource contains over 10 million records and grows by approximately 75,000 new entries each month, ensuring provider profiles remain up-to-date. The system gathers data from 56 U.S. jurisdictions and over 800 taxonomies as new information becomes available. Brenda J. W., CEO of Verisys, emphasized the platform's unique reach:
"Verisys develops substantive information that cannot be found in an OIG, SAM, or licensing searches".
Handling over 2 million outsourced credentialing events annually, Verisys stands out as the only credential verification organization accredited by both NCQA and URAC.
Compliance Monitoring Features
Verisys' VerisysWatch feature offers Continuous True Monitoring, which tracks changes in license status, expirations, and any new sanctions in real time. It goes beyond basic checks by automatically screening national sex offender and abuse registries and conducting real-time verifications against OIG, SAM, Medicare Opt-Out, and PECOS enrollment databases. For NEMT providers managing driver fleets, Verisys ensures compliance by verifying driver’s license numbers, insurance status, and driving history. Additionally, pre-expiration notifications help organizations avoid lapses in driver eligibility, which could lead to fines or liability issues.
Pricing and Affordability
Verisys uses a scalable pricing structure based on the number of credentialing events and the specific datasets required. Organizations can choose to integrate Verisys data with their in-house teams, adopt a hybrid workflow, or fully outsource credentialing to Verisys as a Credential Verification Organization (CVO). By consolidating multiple compliance tools into one system, Verisys can help reduce operational costs. The company also reports that its data is 30% more actionable compared to other solutions on the market. Integration is seamless, whether through a unified API or a custom Salesforce app.
Next, we’ll take a closer look at how Modio Health approaches credential verification for NEMT providers.
6. Modio Health
Modio Health's OneView platform connects with over 250 state, federal, and national credentialing organizations to automatically retrieve real-time primary data. This includes crucial information like DEA registrations, state licenses, NPI numbers, CAQH data, board certifications, and OIG exclusion statuses. By doing so, it helps organizations stay compliant with federal healthcare and Medicaid standards. Additionally, its Universal Provider Record simplifies the verification process, making credentialing tasks more efficient.
Primary Source Verification
The Universal Provider Record consolidates all credentialing data into a single, digital profile for each provider. This eliminates the need for manual spreadsheets and repetitive submissions. Like other top platforms, Modio Health uses automation to reduce administrative workloads while ensuring compliance. With a 4.9/5 user rating from nearly 1,000 companies and a KLAS score of 93.1/100, Modio Health ranks as the top choice for value and performance.
Compliance Monitoring Features
OneView is equipped with automated alerts to notify users when licenses or certifications are nearing expiration. It also tracks CAQH re-attestation dates, providing detailed reports and alerts to ensure compliance is maintained. Mark K., Market Director of Physician Services at Scion Health, shared the impact Modio Health had on their operations:
"Before partnering with your team, credentialing issues were costing us up to $400,000 in lost revenue. Since working with you, we've seen a dramatic improvement in our payer enrollment and claim processing".
The platform is SOC 2 Type II Compliant, which means it undergoes independent audits to ensure top-tier data security. This level of automated monitoring underscores Modio Health's dedication to simplifying compliance for healthcare organizations.
Pricing and Affordability
Modio Health provides tailored pricing based on the number of providers and specific organizational needs. Many organizations report a 75% return on investment, and individual providers can access the Universal Provider Record free of charge. The implementation process includes custom data migration and unlimited training at no extra cost.
sbb-itb-cef70f4
7. Medallion
Medallion is making waves in the credentialing space with its AI-powered automation, streamlining the entire credentialing process from verification to ongoing monitoring. By automating data extraction and standardization from licenses, forms, and PDFs, Medallion eliminates the need for manual templates and speeds up provider intake. Healthcare organizations using Medallion have reported onboarding providers 19 days faster compared to older methods, cutting intake times from 8 days to under 2 hours.
Primary Source Verification
Medallion combines AI technology with human oversight to extract, standardize, and organize data based on specific state requirements. This innovative approach has helped organizations like Headspace cut credentialing time by 60% while maintaining a 95% success rate on credentialing audits. Katie Dave, Director of Partner Operations at Headspace, highlighted the platform's impact:
"Medallion tracks our data and ensures we're compliant with all requirements - it has allowed us to score over 95% on all credentialing audits".
Compliance Monitoring Features
The platform also excels in compliance monitoring, continuously tracking credentials and managing license and certification expirations. It adheres to NCQA, Joint Commission, and CMS standards, offering built-in compliance tracking and automated validations. Tampa General Hospital is a prime example of its effectiveness, saving $2.3 million annually and boosting team efficiency by 90%. Scott Arnold, Executive Vice President & Chief Digital and Innovation Officer, shared:
"The inefficiency we were experiencing was unsustainable. High operating costs and long timelines risked service quality and our competitive edge".
Medallion can prepare credentialing files for committees in as little as three days and has earned a 100% audit score from Optum. These features ensure that providers, including NEMT organizations, stay compliant and ready for audits.
Pricing and Affordability
While Medallion’s pricing structure remains undisclosed, its focus on delivering strong ROI through efficiency and cost savings is clear. The launch of CredAlliance, a national credentialing clearinghouse, is a game-changer. This initiative allows providers to complete credentialing once and share results across multiple payer networks, potentially saving the healthcare system a staggering $1.2 billion annually on redundant credentialing efforts. Organizations using Medallion have reported a 60% reduction in time spent on credentialing tasks, highlighting the platform’s ability to cut both time and costs.
8. CredentialingSpectrum
CredentialingSpectrum is an AI-powered tool designed with affordability in mind, making it a practical choice for small to medium-sized businesses, including NEMT providers working within tighter budgets. Lisa Munger from HealthSource Integrated Solutions shared her experience, stating:
"CredentialingSpectrum cut our enrollment processing time by 40%. We onboard providers faster than ever, streamlining every step with intelligent automation."
Here’s a closer look at the platform’s standout features that simplify credential verification and compliance.
Primary Source Verification
CredentialingSpectrum goes beyond basic OIG sweeps by offering seven layers of source verification. It performs real-time checks against databases like SAM, OFAC, and Medicare/Medicaid exclusion lists. The platform also connects directly with key healthcare data sources such as CAQH ProView, NPDB, FSMB, ABMS, Nursys, and NPPES. This ensures a thorough verification process for both individual providers and groups. To top it off, the platform complies with stringent standards, including HIPAA, SOC 2 Type II, and ISO 27001, while maintaining digital signatures and detailed audit records.
Broker Integration
CredentialingSpectrum simplifies payer enrollment with its Smart Form Mapping and Auto-Fill capabilities, which support various formats like webforms, Excel rosters, and PDFs. Its seamless integration with CAQH ProView has earned user praise. Stephanie from ICMB Services shared:
"Powerful, Impressive and so easy to Use! I liked the way product is integrated with CAQH and Auto form population."
Compliance Monitoring Features
The platform’s AI Command Center and Compliance Knowledge Assistant provide instant answers to regulatory questions and streamline workflows. Automated alerts for expiration and renewal tracking help avoid oversights. Additionally, configurable milestone management tracks credentialing tasks, highlighting what’s completed, overdue, or still in progress. Felicia Browns from UCPG emphasized its usefulness:
"Perfect reminders which helps me everyday to make sure I am on always on it."
Pricing and Affordability
CredentialingSpectrum is priced at just $5 per provider per month, making it highly accessible. The subscription includes a free trial, dashboard analysis, CAQH ProView integration, data source verification, and robust support via email, phone, and a ticketing system.
9. MediRoutes Pro
MediRoutes Pro is a cloud-based solution designed to meet the needs of Non-Emergency Medical Transportation (NEMT) providers, whether they operate a single vehicle or a large fleet. It simplifies dispatch and fleet management while automating credential verification and ensuring compliance with industry regulations. The platform is integrated with leading NEMT brokers across the country, offering a centralized system to improve both operational efficiency and compliance management. Its API-based integrations allow seamless connections with these brokers, eliminating manual processes.
Broker Integration
MediRoutes Pro leverages API-based integrations to connect directly with major NEMT brokers. This enables real-time updates on trips and ensures data synchronization across platforms. Such integration keeps provider information aligned with broker-specific requirements, saving time and reducing errors. A centralized dashboard offers managers instant access to critical data like driver safety reports and fleet performance metrics. Additionally, the dedicated Driver App enhances communication, providing instant status updates and simplifying compliance by tracking driver activities.
Compliance Monitoring Features
The platform ensures all trip data is logged and stored for regulatory reviews and audits, maintaining a comprehensive historical audit trail. Real-time GPS tracking helps monitor vehicle locations and ensure adherence to planned routes. Detailed reports covering driver safety and vehicle maintenance further enhance operational oversight. Digital tools for trip verification, such as signature capture, timekeeping, and passenger notifications, not only support billing accuracy but also help minimize the risk of fraud. By digitizing these processes, MediRoutes Pro eliminates the need for paper records, streamlining workflows and improving record-keeping efficiency.
Pricing and Affordability
MediRoutes Pro does not publicly list its pricing tiers, as the solution is tailored to fit the unique needs of each operation. Its flexibility allows it to scale from small providers with a single vehicle to large fleets with hundreds of vehicles. By operating as a cloud-based system, it eliminates the need for specialized hardware, reducing upfront costs. Accessible from any device, the platform is particularly beneficial for smaller providers looking to minimize infrastructure investments. The software includes customized interfaces for different roles, such as a mobile app for drivers, a web app for dispatchers, and an analytics dashboard for managers.
10. Bambi NEMT Software
Bambi NEMT Software is a cloud-based platform designed to meet the unique needs of Non-Emergency Medical Transportation (NEMT) providers. It automates key tasks like scheduling, routing, and billing while ensuring regulatory compliance. With a bulk upload feature capable of handling anywhere from 10 to 10,000 trips, the system is well-suited for both small operators and larger fleets. The platform’s credential-based scheduling system uses its proprietary Driver & Vehicle Constraints feature to match trips with qualified drivers and properly equipped vehicles, ensuring compliance with certifications. This approach integrates seamlessly with advanced credential verification processes.
Broker Integration
Bambi directly connects with major NEMT brokers such as SafeRide and Modivcare, simplifying trip intake and data exchange. The bulk upload feature processes trip requests from brokers and care facilities efficiently. By leveraging the Driver & Vehicle Constraints system, the software ensures that trips are only assigned to compliant drivers and vehicles. Additionally, real-time driver-dispatch chat and notifications help maintain smooth operations and meet broker expectations.
Compliance Monitoring Features
Built on a HIPAA-compliant framework, Bambi offers encrypted data storage, role-based access controls, and detailed audit trails that log who accessed information and when. This ensures transparency during regulatory reviews. The platform also supports electronic service attestation using GPS-based timestamps and e-signatures. For added safety, its dedicated mobile driver app includes a Pre-Shift Vehicle Inspection tool, which digitizes safety checks and creates clear vehicle readiness records.
Pricing and Affordability
Pricing details for Bambi are available upon request through a demo. The platform offers customized plans tailored to operational needs. It includes an Advance Pricing Rule tool, allowing providers to set up personalized pricing structures. With built-in credit card processing and invoice generation, payment collection becomes more efficient. As a cloud-based solution, Bambi eliminates the need for costly hardware, making it an appealing option for providers aiming to reduce upfront infrastructure expenses.
Tool Comparison Table
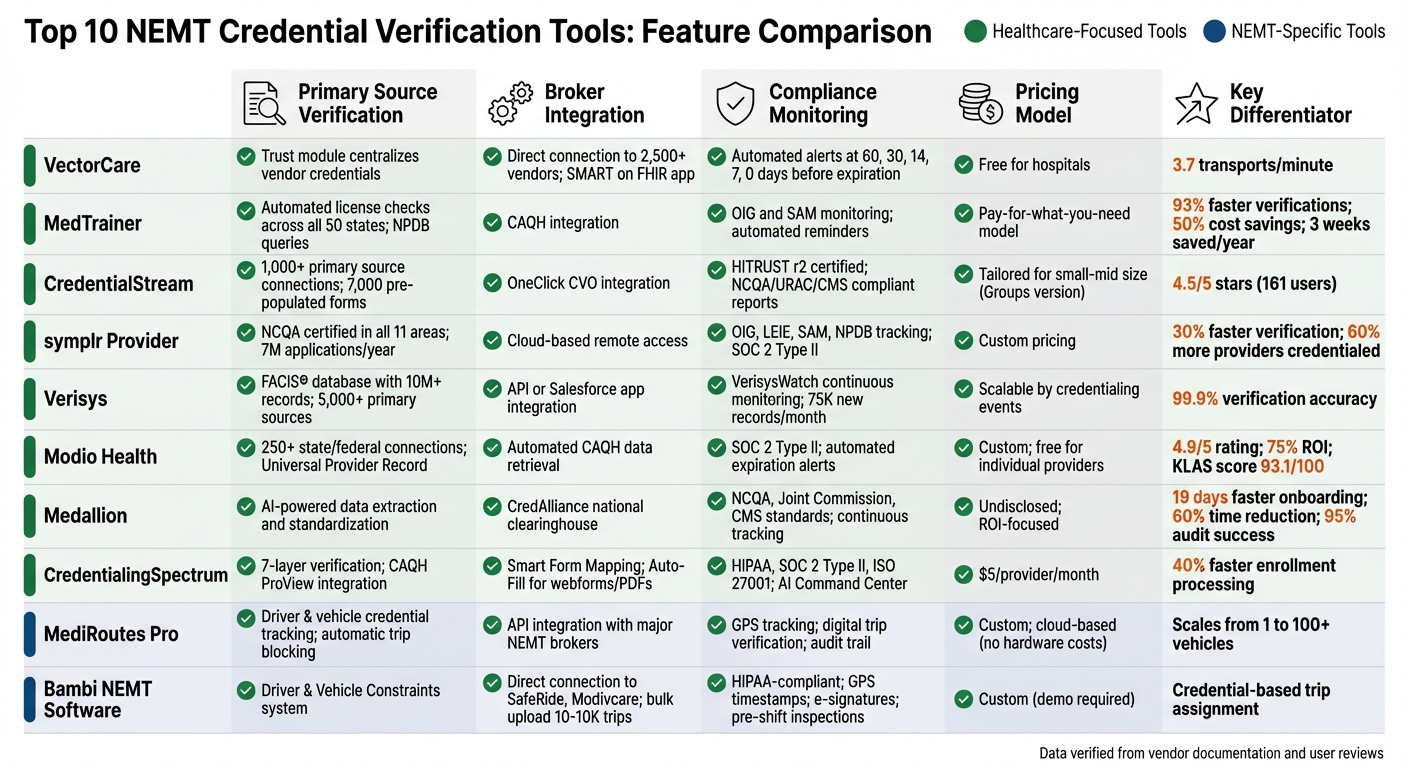
Top 10 NEMT Credential Verification Tools Feature Comparison
Selecting the right credential verification tool for your NEMT operation hinges on factors like your organization's size, budget, and compliance requirements. Here's a quick breakdown of verified features for various tools:
| Tool | Primary Source Verification | Broker Integration | Compliance Monitoring | Pricing |
|---|---|---|---|---|
| VectorCare | ||||
| MedTrainer | ||||
| CredentialStream | ||||
| symplr Provider | ||||
| Verisys | Database of 10M+ records for sanctions and provider data | API integration for health plans | OIG and state-level exclusion monitoring | |
| Modio Health | ||||
| Medallion | ||||
| CredentialingSpectrum | Time-stamped screenshots from governing boards | |||
| MediRoutes Pro | Driver and vehicle credential tracking; automatic trip blocking for expired credentials | |||
| Bambi NEMT Software |
This table outlines the key features of each tool, helping you align your choice with your operational needs. For smaller providers, tools with lower upfront costs are often ideal. Larger fleets typically require enterprise-level systems with robust API capabilities, while mid-sized operations may benefit most from NEMT-specific tools that combine credentialing with trip management.
Notably, tools tailored for NEMT streamline credentialing for drivers, vehicles, and providers, focusing on operational needs. In contrast, broader healthcare tools often emphasize extensive data integration and compliance monitoring.
"Being able to have that real-time access to credentialing status in Salesforce and having it be so easy to use and understand, is huge for us." – Holly Long, Director of Operations
When assessing cost-effectiveness, consider the balance between per-transaction fees and the time saved through automation. Automated tools can significantly reduce administrative workload. Additionally, tools that provide time-stamped primary source screenshots are invaluable for regulatory reviews and broker audits, ensuring you’re always audit-ready.
Conclusion
Credential verification tools bring measurable improvements in efficiency and compliance for NEMT providers. Automated credentialing software can cut payer enrollment time by 60% and save around three weeks annually on administrative tasks. This ensures that only qualified drivers and vehicles handle trips, while also protecting your revenue cycle from disruptions.
Studies reveal that 93% of users experience faster primary source verifications and exclusion checks with specialized software. Additionally, 95% of license verifications are completed within just two days. Such speed is essential for staying on top of driver certifications, vehicle inspections, and insurance requirements, especially under Medicaid's $1.5 million liability mandate. Real-time monitoring against OIG and SAM databases further helps providers avoid legal penalties and maintain audit-ready records.
Here’s what users are saying:
"MedTrainer saves us time and money on employee verifications and exclusion checks." – Tish Woodall, Administrator, Tri-State Community Health Center
When selecting a credentialing tool, consider your operation’s size and needs. Smaller providers often benefit from straightforward, cost-efficient platforms, while larger fleets may require enterprise-level systems with advanced API integrations. For mid-sized operations, NEMT-specific tools that combine credentialing with trip management can offer excellent value. Look for platforms that integrate smoothly with your scheduling and billing systems to prevent data silos and ensure seamless operations as your business grows.
Key features to prioritize include automated 30-day expiration alerts, primary source screenshots for audits, and continuous exclusion monitoring. With the NEMT industry expected to hit $12 billion by 2028, choosing the right credentialing platform now can set your business on a path to long-term success. By balancing compliance with efficiency, these tools not only safeguard patient safety but also position your business for growth in a competitive market.
FAQs
How can automated credential verification tools help NEMT providers stay compliant?
Automated credential verification tools make compliance much easier by turning tedious manual tasks into real-time, seamless checks. These tools handle licenses, vehicle inspections, insurance, training, and certifications by pulling data straight from reliable sources. This not only ensures data accuracy but also cuts down on errors. Plus, they offer ongoing monitoring and send automatic alerts for upcoming expirations, giving providers enough time to resolve potential issues before they become compliance problems.
By keeping all records current and ready for audits, these tools help NEMT providers meet the standards set by NCQA, The Joint Commission, and state regulations. This proactive system lightens the administrative load, prevents eligibility lapses, and ensures smoother audits - all while prioritizing patient safety and keeping operations running efficiently.
What should a small NEMT business consider when choosing a credential verification tool?
When choosing a credential verification tool for your small NEMT business, focus on key features like automation, accuracy, compliance, and integration. Automated tools can save you hours of manual work by delivering results in seconds, cutting credentialing delays by as much as 98%. Make sure the tool adheres to industry standards, such as NCQA or URAC certifications, and includes compliance monitoring to keep you aligned with federal and state regulations.
It's also important to find a tool that integrates smoothly with your existing systems, such as scheduling or dispatch platforms, to ensure your workflows remain uninterrupted. Budget considerations matter too - opt for solutions with transparent, pay-as-you-go pricing to manage costs effectively while still getting dependable results. Features like ongoing monitoring, easy-to-navigate dashboards, and thorough background checks can further simplify your processes and support your business as it grows.
How do credential verification tools connect with scheduling and billing systems in NEMT?
Credential verification tools for NEMT are designed to work effortlessly with your current scheduling and billing systems. Many of these tools rely on RESTful APIs or webhooks to deliver real-time updates on key credentials, such as driver licenses, insurance policies, and training expiration dates. This means scheduling systems can automatically restrict access to drivers or vehicles that fall short of compliance standards, ensuring that only qualified providers are assigned to trips.
Some tools go a step further by offering built-in integrations with major broker platforms like ModivCare and MTM. These integrations synchronize credential data with scheduling and Medicaid billing workflows, cutting down on manual data entry and reducing the chance of errors. By linking credential data directly to dispatch and billing systems, these tools not only simplify operations but also help NEMT providers stay aligned with regulatory requirements.


