

NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Private Pay NEMT businesses typically see higher profit margins (20%-30%) compared to Medicaid NEMT (10%-15%). While Medicaid offers steady demand from 3–4 million beneficiaries annually, reimbursement delays (30–90 days) strain cash flow. Private Pay, with faster payments (1–7 days) and higher trip rates ($75–$150 vs. Medicaid’s $40–$60), provides better cash flow but requires active marketing and client relationships.
Key differences:
- Revenue per trip: Private Pay is higher.
- Cash flow: Private Pay benefits from immediate payments.
- Profitability: Private Pay has higher margins but depends on economic stability.
- Demand: Medicaid offers consistent volume; Private Pay fluctuates with market trends.
Quick Comparison:
| Feature | Medicaid NEMT | Private Pay NEMT |
|---|---|---|
| Revenue per Trip | Lower ($40–$60) | Higher ($75–$150) |
| Profit Margins | 10%–15% | 20%–30% |
| Payment Timelines | 30–90 days | 1–7 days |
| Demand Stability | Consistent | Market-dependent |
| Startup Costs | Lower | Higher (specialized vehicles) |
Choosing the right model depends on your market, resources, and risk tolerance. A balanced approach combining both models can stabilize cash flow while maximizing revenue.
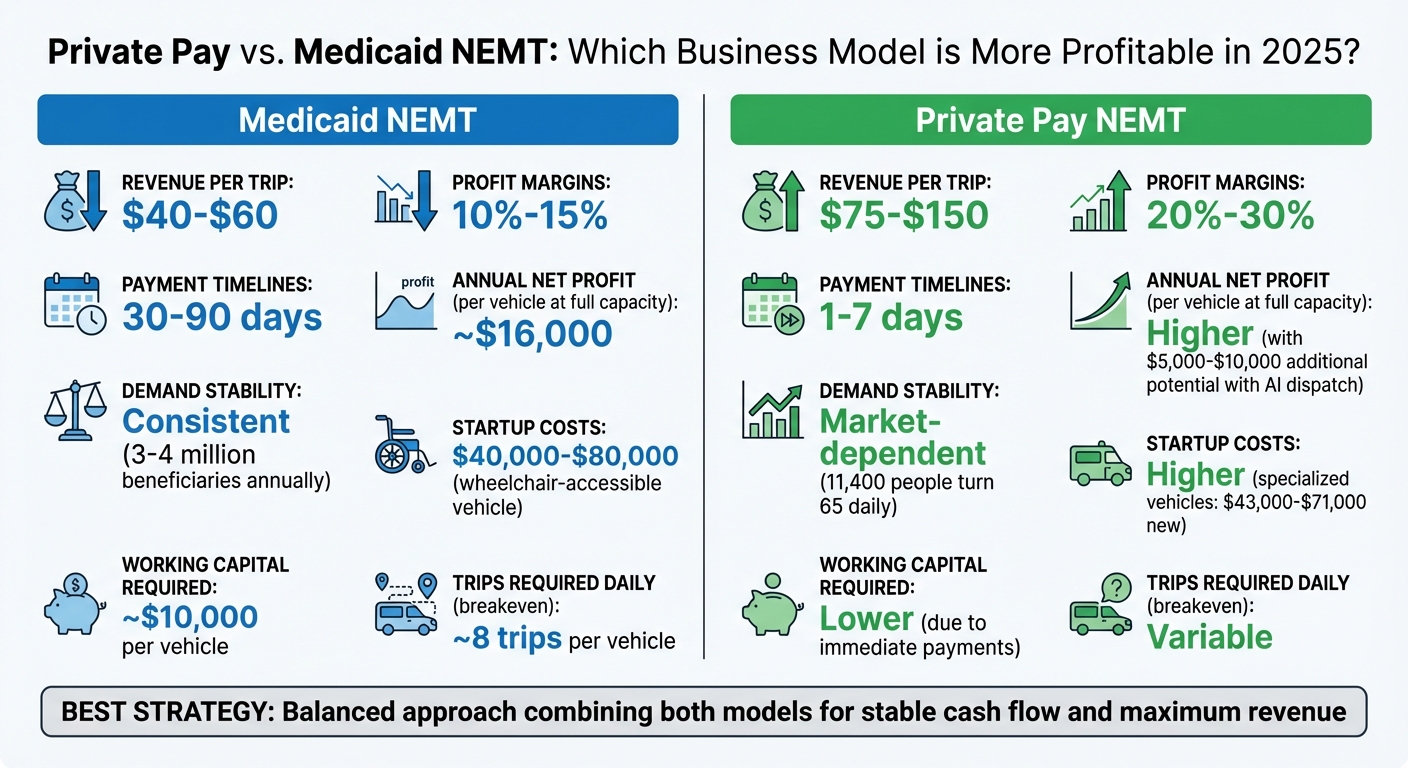
Private Pay vs Medicaid NEMT Business Model Comparison 2025
Medicaid NEMT Business Model
Revenue Structure
Medicaid Non-Emergency Medical Transportation (NEMT) providers earn revenue through state-run programs, which operate under four main delivery models: Brokerage (capitated funding), Managed Care Organization (MCO), Mixed, and In-house (fee-for-service). Payments are typically structured around mileage reimbursements - ranging from $2.00 to $4.00 per mile - or hourly rates between $25.00 and $60.00 per hour. A single vehicle operating at full capacity can bring in $50,000 to $60,000 annually.
The financial dynamics differ depending on the state and the chosen delivery model. Per Member Per Month (PMPM) costs, which represent the amount states pay to administer NEMT benefits, vary widely - from as low as $0.72 in some Managed Care states to $16.57 in states that rely heavily on Brokerage models. Most trips are relatively short, with 75% covering less than 10 miles and 90% staying under 20 miles. This means that providers must concentrate on achieving high trip density to maximize their revenue. These figures provide a foundation for assessing profitability in the Medicaid NEMT sector.
Profitability Profile
A Medicaid NEMT vehicle running at full capacity typically generates an annual net profit of around $16,000. This modest return reflects the tight margins created by fixed reimbursement rates and variable operating costs. For example, fuel costs average $0.20 per mile, while maintenance expenses are about $0.12 per mile.
Cash flow is another significant hurdle. Each vehicle requires at least $10,000 in working capital to cover upfront costs like fuel, maintenance, and driver wages, which average $28,500 annually. Since Medicaid payments are often delayed by a month or more, operators frequently rely on credit or personal savings to bridge the gap, further straining profitability.
Operational Requirements and Market Risks
Running a Medicaid NEMT business involves meeting strict compliance standards. For instance, operators are required to implement GPS tracking and electronic scheduling systems, which cost approximately $50 per vehicle per month. Other challenges include no-show appointments and low trip density in rural areas, which can disrupt efficiency and revenue generation. Setting up a single wheelchair-accessible vehicle, including its purchase and necessary working capital, typically costs between $40,000 and $80,000.
"A challenge faced by many states is maintaining program integrity and overseeing vendor relationships."
Providers also face geographic coverage requirements that may compel them to serve rural areas with low trip volumes, where operational costs often outweigh revenue.
Looking ahead to 2024–2025, trends show a growing preference for Managed Care models, as seen in Nebraska’s 2019 transition from direct brokerage to MCO contracts. While this shift has generally reduced PMPM costs, it has also introduced stricter oversight. According to Milliman:
"Wide variance in margins for service providers and quality of experience for beneficiaries"
illustrates how profitability is closely tied to a state’s delivery model and reimbursement structure. These factors highlight the importance of carefully balancing revenue opportunities against operational risks when evaluating Medicaid NEMT business models.
Private Pay NEMT Business Model
Revenue Structure
Private pay Non-Emergency Medical Transportation (NEMT) providers operate by charging clients or facilities directly, skipping broker intermediaries. Their pricing typically includes a base fare - around $45 to $50 for wheelchair trips - plus per-mile fees of $3 to $5, and wait time charges ranging from $15 to $30 for every 30 minutes. Premium services like dialysis or stretcher transportation command higher rates. For example, dialysis trips can bring in $75 to $150 per trip, compared to Medicaid's $40 to $60. Stretcher or gurney transport often starts with base fees of $100 to $200, with mileage rates climbing to $5 to $10 per mile. Pricing varies by location, with urban areas generally charging more than rural ones.
Recurring contracts with nursing homes, retirement communities, and dialysis centers provide a steady stream of income. These agreements not only stabilize revenue but also reduce the need for ongoing marketing efforts to maintain a full schedule. This direct-pay structure offers a more lucrative revenue model compared to operations reliant on Medicaid reimbursements.
Profitability Profile
Thanks to their pricing flexibility and faster payment cycles, private pay NEMT providers typically enjoy higher profit margins - 20% to 30% - compared to Medicaid's 10% to 15%. Payments from private clients are settled quickly, often within one to seven days, unlike Medicaid reimbursements, which can take 30 to 90 days. This faster cash flow reduces the need for large working capital reserves, allowing providers to reinvest earnings and expand their operations more efficiently.
"Private pay clients represent your most profitable stream. Direct payment eliminates broker fees and accelerates payment to same-day or within 7 days." - EliteMed Financials
Adopting AI-powered dispatch software can further boost profitability. By increasing vehicle utilization rates from an industry average of 35% to as high as 60% to 80%, providers can generate an extra $5,000 to $10,000 per vehicle annually. This technology also minimizes "deadhead" miles - empty trips that can cut into profits by as much as 20% to 30%.
Operational Requirements and Market Risks
Success in the private pay model hinges on strong relationships with clients and facilities. Unlike broker-driven models, private pay providers must actively engage with caregivers, facility administrators, and individual clients. Delivering consistent, high-quality service is essential; poor performance, such as delayed pickups or equipment failures, can quickly damage trust.
Demographic trends favor the private pay model, with a growing senior population driving demand. By 2025, approximately 11,400 people will turn 65 each day, and about 4 million Americans annually miss or delay medical appointments due to transportation challenges. However, this demand is sensitive to economic conditions, as customers may postpone non-urgent trips during financial downturns.
In competitive urban areas, standing out requires investments in specialized equipment like wheelchair lifts or bariatric-capable vehicles, along with enhanced features such as real-time GPS tracking. While the initial cost of wheelchair-accessible vehicles is steep - ranging from $43,000 to $71,000 for new models and $16,000 to $83,000 for used ones - strategic contracts with facilities can help offset these expenses and reduce financial risks.
Profitability Comparison: Private Pay vs. Medicaid NEMT
Economic Drivers Comparison
The financial dynamics of Medicaid and private pay NEMT models are strikingly different. Medicaid NEMT often operates on narrow margins, relying heavily on high trip volumes to sustain profitability. On the other hand, private pay services charge higher rates per trip and benefit from immediate payments, which significantly reduces cash-flow challenges. For Medicaid providers, payment delays of 30 to 60 days - or even longer - mean they need nearly $10,000 in working capital per vehicle just to cover ongoing expenses like fuel, maintenance, and wages. In contrast, private pay providers receive payment at the time of service, allowing for smoother cash flow.
| Feature | Medicaid NEMT Model | Private Pay NEMT Model |
|---|---|---|
| Revenue per Trip | Lower (state or broker contract rates) | Higher (market-driven premium rates) |
| Profit Margins | Tight; dependent on trip volume | Generally higher margins |
| Payment Timelines | Delayed (30–60+ days) | Immediate payment at service |
| Cash-Flow Stability | Lower; requires substantial working capital | Higher; benefits from instant revenue |
| Trip Volume Required | Around 8 trips per day per vehicle | Variable, based on market conditions |
"You will likely have to cover fuel, maintenance, driver wages and other expenses for at least a month before you start to get paid by Medicaid."
– Adam Hoeksema, Co-founder, ProjectionHub
These differences in revenue streams directly influence operational costs and overall business strategies.
Cost and Operations Analysis
The revenue models of Medicaid and private pay NEMT providers naturally shape their operational costs. Medicaid providers, for example, often invest in specialized software for routing and dispatching - costing about $50 per vehicle monthly - to handle the high trip volumes required to break even. Each vehicle typically needs to complete around 8 trips daily just to cover fixed operating costs.
Private pay providers, while facing higher customer acquisition costs and potential investments in specialized equipment, benefit from higher per-trip revenues and immediate payments. This offsets their upfront expenses. Additionally, while private pay operations face less stringent regulatory oversight compared to Medicaid, they must maintain excellent service quality to retain contracts with facilities and individual clients.
Operational costs aside, market demand also plays a critical role in shaping the potential of these business models.
Market Demand and Growth Outlook
Market trends further highlight the strengths and challenges of each NEMT model. The overall NEMT industry is projected to grow from $8.66 billion in 2021 to approximately $15.58 billion by 2028. Medicaid NEMT enjoys consistent, recurring demand. Around 4% to 5% of Medicaid beneficiaries - roughly 3 to 4 million people - use these services regularly. High-need groups, including dialysis patients, individuals with intellectual disabilities, and those undergoing treatment for substance use disorders, drive significant trip volumes. Interestingly, Medicaid ride volumes in 2021 were about 30% lower than pre-pandemic levels, suggesting room for recovery and growth as the healthcare sector stabilizes.
Private pay NEMT demand, on the other hand, is more closely tied to overall healthcare consumption patterns. While this model is somewhat more vulnerable to economic shifts, its pricing flexibility allows providers to adapt to market needs. As preventive care and chronic condition management become more prominent, private pay services are well-positioned to meet the evolving demands of healthcare consumers.
sbb-itb-cef70f4
Choosing the Right NEMT Payer Strategy for Your Business
Assessing Your Local Market
Start by understanding your state’s NEMT (Non-Emergency Medical Transportation) delivery model. Does your state operate under a brokerage system, Managed Care Organization (MCO), a mix of models, or a fee-for-service structure? This will shape how you contract for services, process payments, and manage trips.
Medicaid costs vary widely by state. For example, Per Member Per Month (PMPM) expenses can range from $0.72 to $16.57, depending on the state and delivery model. States with higher PMPM costs often serve populations with greater medical needs, such as the elderly, disabled, or those in managed long-term care programs. These states may offer better reimbursement rates but often require stricter compliance with oversight regulations.
To determine your business’s viability, perform a breakeven analysis. Factor in local startup costs, operational expenses, and expected revenue, which typically falls between $2 and $4 per mile. Consider that around 75% of NEMT trips are under 10 miles, and a single vehicle usually completes about 8 trips daily. If you’re entering a market with fewer competitors, you might benefit from higher reimbursement rates due to reduced competition. This analysis will help you establish a strong foundation for optimizing your payer mix.
Designing a Profitable Payer Mix
A balanced payer mix is key to maintaining steady cash flow and healthy margins. Combining Medicaid contracts with private pay options can help achieve this balance. Medicaid offers consistent, high-volume demand, but payments can be delayed. On the other hand, private pay trips often come with higher rates and quicker payments, which can offset Medicaid’s slower cash flow.
In states with mixed delivery models, consider working with both MCOs and state contracts to expand your market reach. With about 74% of Medicaid beneficiaries enrolled in Managed Care programs as of 2021, it’s important to know whether NEMT services are "carved in" (managed by health plans) or "carved out" (handled separately by the state). This knowledge will guide you in identifying the best partners for your services.
Investing in technology can also improve your operations and compliance. Many states now require GPS tracking and electronic scheduling systems to prevent fraud and monitor vendor performance. Implementing these tools early - at an estimated cost of $50 or more per vehicle each month - can help you meet regulatory requirements while streamlining your operations.
Role of Industry Insights
To stay profitable, it’s essential to keep up with industry trends and changes. The NEMT landscape is constantly shifting as states update delivery models, reimbursement rates, and oversight policies. Staying informed allows you to adjust your payer strategy proactively instead of scrambling to react to challenges.
Resources like NEMT Entrepreneur can provide valuable, up-to-date insights. Whether you’re analyzing state-specific PMPM data, tracking new regulations, or planning for growth, having access to timely information can help you make smarter decisions, seize opportunities, and avoid costly mistakes.
Lucrative On-Demand NEMT for Facilities, with the CEO of Roundtrip | NEMT Experts Podcast Episode 62
Conclusion
Deciding between Medicaid and private pay NEMT models in 2025 comes down to understanding what aligns best with your market and operational goals. Medicaid provides steady volume, serving around 3–4 million beneficiaries annually, but it often involves delayed payments and varying reimbursement rates across states. On the other hand, private pay models require active marketing efforts and managing fluctuations in demand.
The most successful NEMT providers in 2025 won’t rely solely on one payer source. Instead, they create a balanced mix that combines Medicaid's consistent volume with additional revenue streams to maintain cash flow and boost profitability. Tailoring this mix to your state’s delivery model, competitive environment, and target demographics is key. This approach builds on the comparisons highlighted earlier.
Investing in tools like GPS tracking and electronic scheduling (typically around $50 per vehicle per month) can help meet compliance standards, minimize cancellations, and secure more lucrative contracts. These tools complement the earlier discussion on balancing revenue streams and operational expenses.
With the NEMT market expected to grow from $8.66 billion in 2021 to $15.58 billion by 2028, the opportunities are substantial. Success will hinge on understanding local market dynamics, maintaining sufficient working capital, and staying up-to-date with changing regulations and reimbursement policies.
Use these insights to evaluate your state’s PMPM costs, delivery model, and competitive landscape. Build a payer strategy that aligns with your financial and operational capabilities, and adjust your approach as you analyze performance data over time.
FAQs
What makes the Private Pay NEMT model more profitable than Medicaid NEMT?
The Private Pay NEMT model brings several key advantages that can boost profitability compared to Medicaid-based transportation. One major benefit is quicker payment turnaround. Since riders pay directly, providers often receive payments the same day or within 30 days, unlike Medicaid reimbursements, which can take anywhere from 30 to 90 days. This faster cash flow can significantly improve a provider's financial stability.
Another advantage is the ability to set your own rates. Unlike Medicaid's fixed reimbursement rates, Private Pay allows providers to charge higher rates, leading to better profit margins per trip. On top of that, the administrative burden is much lighter. Private Pay trips require only basic invoicing, eliminating the need for the extensive documentation and claims process that Medicaid billing demands.
With faster payments, greater pricing flexibility, and reduced paperwork, the Private Pay model offers NEMT providers a simpler and potentially more profitable path in 2025.
What’s the best way for NEMT providers to balance the benefits and challenges of combining Private Pay and Medicaid models?
To effectively manage both Private Pay and Medicaid models, NEMT providers can capitalize on the distinct advantages each offers. Private Pay typically delivers quicker cash flow - ranging from immediate payments to within 30 days - and allows for higher, market-driven rates. However, it requires consistent marketing efforts and can be less predictable. On the flip side, Medicaid ensures steady, government-backed income but comes with lower reimbursement rates, longer payment cycles (30–90 days), and additional administrative tasks.
A balanced approach might involve allocating part of your fleet and resources to Medicaid for consistent revenue, while reserving some capacity for Private Pay to capture higher profit margins. To manage Medicaid's slower payments, consider using automated billing tools to simplify processes and maintaining a cash reserve - enough to cover 1–2 months of expenses. For Private Pay, implementing a straightforward online booking system and running cost-effective marketing campaigns can help attract clients without breaking the bank.
Regularly assessing your client mix and staying attuned to market trends is key. If demand for Private Pay services grows, you can adjust resources to boost profitability while relying on Medicaid for financial stability. This adaptable strategy creates a business model that’s both secure and lucrative.
What key technologies can help boost profitability in the NEMT business?
To run a profitable NEMT business, investing in the right technologies is a game-changer. For starters, a cloud-based dispatch system can take the hassle out of scheduling. It automates the process, matches drivers with nearby requests, and optimizes routes. The result? Lower fuel and labor costs, plus better use of your vehicles.
Next, billing and claims software is a must-have. It simplifies Medicaid reimbursements by generating compliant claims and tracking payments. This means fewer delays and a smoother cash flow.
Other tools worth considering include GPS telematics and driver-monitoring apps. These provide valuable insights into fuel consumption, idle times, and vehicle health. With this data, you can schedule preventive maintenance and avoid unexpected downtime. On the customer side, mobile rider apps offering real-time ETAs, pickup confirmations, and electronic signatures can elevate the rider experience and justify higher private-pay rates.
Finally, integrating dispatch systems with electronic health records (EHRs) can streamline operations even further. Accurate eligibility checks and seamless data sharing cut down on administrative work, making your operation more efficient. Together, these technologies can transform your NEMT business into a more efficient and profitable venture.


