NEMT Entrepreneur provides expert insights, strategies, and resources to help non-emergency medical transportation professionals grow their businesses. Get industry-leading advice to succeed in NEMT.
Featured articles
Are you unknowingly violating HIPAA rules as an NEMT dispatcher? Mishandling sensitive patient information can lead to hefty fines, legal scrutiny, and a damaged reputation. Here's what you need to know:
- NEMT dispatchers are classified as Business Associates under HIPAA, meaning they must safeguard Protected Health Information (PHI).
- Common mistakes, like sharing patient details via unsecured devices or accessing unnecessary PHI, can result in violations.
- Penalties range from $137 to $2,067,813 per violation, depending on intent and corrective actions.
- Dispatchers must sign Business Associate Agreements (BAAs) with healthcare clients and vendors to legally handle PHI.
To stay compliant:
- Use HIPAA-compliant software with encryption and role-based access controls.
- Limit PHI access to the minimum required for tasks.
- Train dispatchers on secure communication, device usage, and breach protocols.
HIPAA compliance isn't just about avoiding fines - it's about protecting patient trust and ensuring your operations run smoothly. Read on for actionable steps to safeguard your NEMT dispatch processes.
HIPAA Compliance for NEMT Providers: Protect Your Business & Avoid Costly Fines!
sbb-itb-cef70f4
What Dispatchers Need to Know About HIPAA Compliance

HIPAA Violation Penalty Tiers and Fine Ranges for NEMT Dispatchers
How Dispatchers Are Classified as Business Associates Under HIPAA
NEMT dispatchers fall under the category of Business Associates because they handle sensitive patient information on behalf of healthcare providers, hospitals, and health plans. The Office for Civil Rights (OCR) defines a Business Associate as "a person or entity that performs certain functions or activities that involve the use or disclosure of protected health information on behalf of, or provides services to, a covered entity".
This classification carries direct legal accountability. Since the passage of the HITECH Act and the 2013 Omnibus Final Rule, Business Associates are subject to the same enforcement standards as healthcare providers. To comply, dispatchers must sign a Business Associate Agreement (BAA) with every healthcare client before accessing any patient data. This requirement doesn’t stop there - if you use third-party software or collaborate with independent drivers who handle PHI, you’ll need separate BAAs with these vendors as well.
Now, let’s take a closer look at the types of PHI dispatchers regularly handle.
Types of PHI Dispatchers Handle Daily
Dispatchers encounter a wide range of protected health information (PHI) during their shifts. This goes far beyond basic scheduling details and includes highly sensitive data.
| PHI Type | Examples Dispatchers Handle |
|---|---|
| Names | Full patient names for trip coordination |
| Geographic Data | Pickup/drop-off addresses, zip codes |
| Dates | Birthdates, appointment times, transport dates |
| Contact Information | Phone numbers for trip confirmations |
| Health Insurance Numbers | Medicaid IDs, beneficiary numbers |
| Medical Conditions | Wheelchair needs, mobility limitations, stretcher requirements |
| Account Numbers | Billing and payment details |
There are 18 specific identifiers that, when combined with health information, classify as PHI. Even small details, like a vehicle’s license plate number, could count as PHI depending on the context. To stay compliant, dispatchers must follow the Minimum Necessary Rule, ensuring they only access the PHI required to complete a transport.
Handling this information improperly can lead to serious legal and financial consequences.
Legal and Financial Penalties for HIPAA Violations
HIPAA violations come with steep penalties, structured across four tiers based on the level of responsibility. These fines, adjusted for inflation, range from $137 to $68,928 per violation, with annual penalties capped at $2,067,813.
| Violation Tier | Minimum Penalty | Maximum Penalty |
|---|---|---|
| Tier 1: Unaware | $137 | $68,928 |
| Tier 2: Reasonable Cause | $1,379 | $68,928 |
| Tier 3: Willful Neglect (Corrected) | $13,785 | $68,928 |
| Tier 4: Willful Neglect (Not Corrected) | $68,928 | $2,067,813 |
Real-world cases illustrate the risks. In 2016, Banner Health was fined $1.25 million after failing to conduct a proper risk analysis, while Cignet Health faced a $4.3 million fine for denying patients timely access to their records.
"Business associates are directly liable for HIPAA violations... [including] failure to make reasonable efforts to limit PHI to the minimum necessary to accomplish the intended purpose." – HHS Office for Civil Rights
Violations can result in more than just fines. They may lead to job loss or even criminal charges for individuals who improperly access sensitive records.
5 Common HIPAA Violations in NEMT Dispatch Operations
HIPAA violations in Non-Emergency Medical Transportation (NEMT) dispatch operations often happen unintentionally. Dispatchers may not realize their actions breach patient privacy, but the consequences can still be severe. By identifying common pitfalls, you can take proactive steps to protect sensitive patient information and avoid costly penalties.
Accessing More PHI Than Needed
Dispatchers should only access the minimum necessary Protected Health Information (PHI) required to perform their duties. For instance, if a dispatcher only needs a patient’s name, pickup location, and mobility requirements to coordinate a ride, viewing their full medical history is a clear violation of HIPAA’s Minimum Necessary standard.
Other common mistakes include discussing patient details with coworkers who don’t need to know or leaving computers unlocked, potentially exposing PHI to unauthorized individuals. To address these risks:
- Use role-based access controls in compliant dispatch software to limit what information each employee can view.
- Ensure computers automatically log off after periods of inactivity and remain password-protected.
- Restrict access to PHI strictly to those with a legitimate need-to-know.
Next, let’s consider the risks associated with unsecured devices.
Using Unsecured Devices for Dispatch Tasks
Personal devices like phones, tablets, or laptops are convenient but can pose serious HIPAA risks if not properly secured. For example, standard SMS lacks encryption, leaving PHI vulnerable during transmission. Additionally, apps on personal devices may collect data, potentially exposing patient locations or visit histories without your knowledge.
"The HIPAA Rules generally do not protect the privacy or security of your health information when it is accessed through or stored on your personal cell phones or tablets."
To minimize these risks:
- Use HIPAA-compliant messaging platforms instead of standard SMS. These platforms should include encryption, automatic session timeouts, and audit trails.
- Disable location services for non-essential apps and remove advertising IDs to prevent third-party tracking.
- Enable remote wiping features on devices to protect data if they’re lost or stolen.
- Require strong user authentication, such as multi-factor authentication, for any device accessing dispatch logs or patient data.
While device security is crucial, tracking how PHI is accessed is equally important.
Failing to Track PHI Access and Maintain Audit Trails
HIPAA requires organizations to track and monitor access to electronic PHI. This includes logging user IDs, timestamps, and actions taken within systems containing sensitive data. Without these audit trails, it’s nearly impossible to determine who accessed patient information, when, or why. For example, in August 2025, 58 healthcare data breaches affected nearly 3.8 million individuals, with 31% of incidents involving compromised user or administrative accounts.
To stay compliant:
- Implement audit controls - whether through software, hardware, or processes - that log every instance of PHI access.
- Regularly review audit logs to identify unusual activity and address potential issues promptly.
Audit trails are a critical tool for detecting and resolving compliance gaps.
Missing Business Associate Agreements (BAAs)
If third-party vendors, contractors, or software providers handle PHI on your behalf, they must sign a Business Associate Agreement (BAA) before accessing any data. Without these agreements, your organization could be held liable for their HIPAA violations. A BAA should outline how the vendor will protect PHI, restrict its use to authorized purposes, report breaches promptly, and either return or destroy PHI when the relationship ends.
To ensure compliance:
- Verify that all vendors handling PHI have signed current BAAs.
- Regularly review and update these agreements to address any changes in services or regulations.
Even one missing BAA can leave your organization vulnerable to compliance issues.
Providing Generic HIPAA Training Instead of Dispatcher-Specific Education
Generic HIPAA training often overlooks the unique responsibilities and risks faced by dispatchers. For example, dispatchers may not realize that using non-compliant messaging apps or accessing patient records without a valid reason violates HIPAA.
"OCR continues to receive complaints about health care providers disclosing their patients' protected health information on social media or the internet in response to negative reviews. Simply put, this is not allowed."
To address this gap:
- Develop dispatcher-specific training that focuses on their daily tasks, such as using mobile dispatch apps, managing trip logs, and securely communicating patient locations.
- Include guidance on avoiding non-compliant tools, recognizing phishing attempts, and responding to suspected breaches.
- Emphasize secure device practices, like not saving PHI locally or using personal cloud storage.
Providing tailored training ensures dispatchers understand their role in maintaining HIPAA compliance and protecting patient privacy.
How to Ensure HIPAA Compliance for Dispatchers
To address common HIPAA challenges, a strong three-layered approach is essential. This includes administrative, physical, and technical safeguards to protect patient information effectively.
Setting Up Administrative, Physical, and Technical Safeguards
HIPAA compliance requires a thorough strategy to secure electronic Protected Health Information (ePHI). Start with a risk analysis using the HHS Security Risk Assessment Tool to identify potential vulnerabilities in your system. After pinpointing risks, appoint a security official responsible for implementing HIPAA policies.
It's crucial to document key procedures such as access management, dispatcher-specific training, and contingency plans for data backup and recovery. Keep this documentation for a minimum of six years from the date it was created or last updated.
For physical safeguards, control access to your dispatch office and workstations by limiting it to authorized personnel. Ensure workstations are positioned to prevent unauthorized viewing and require devices to lock when unattended. When disposing of old hardware or media containing ePHI, follow secure methods - deleting files alone is insufficient.
On the technical side, implement digital defenses like unique user IDs, automatic log-offs, and encryption for all transmitted ePHI. These measures ensure patient data is accessed only by authorized individuals and remains secure during transmission.
"The Security Rule is designed to be flexible, scalable, and technology neutral, enabling a regulated entity to implement policies, procedures, and technologies that are appropriate for the entity's particular size, organizational structure, and risks to ePHI." - HHS
Once these safeguards are in place, refine access further with role-based controls.
Creating Role-Based Access Controls
Role-based access control (RBAC) ensures compliance with HIPAA's "minimum necessary" standard by limiting access to only what each staff member needs for their role. For example, a dispatcher managing transportation may only need to see a patient's name, pickup location, and mobility requirements, while a billing clerk may require access to insurance details but not trip-specific information. This approach reduces the risk of unauthorized access or misuse of data.
Strengthen RBAC with authentication procedures to verify user identities before granting access. Enable audit logging to monitor who accessed specific data and when. Regularly review these permissions - at least every quarter - to ensure they align with current job roles and organizational needs.
Finally, choose dispatch software that supports these controls effectively.
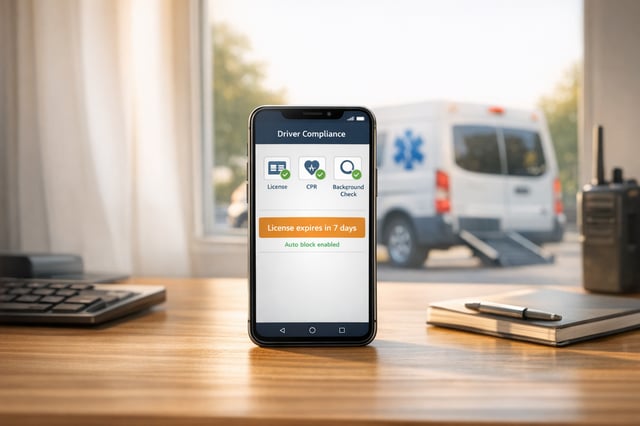
Choosing HIPAA-Compliant Dispatch Software
The dispatch software you select plays a critical role in maintaining HIPAA compliance. Before anything else, confirm that the vendor is willing to sign a Business Associate Agreement (BAA) - this legal agreement is non-negotiable for handling PHI.
During testing, evaluate the software's role-based access features. Ensure it restricts dispatchers from viewing unnecessary medical details while allowing them to schedule transport efficiently. Look for features like automatic data backups for disaster recovery and detailed audit trails to support quarterly compliance reviews. Additionally, software that integrates with existing Electronic Health Records or practice management systems can help reduce errors and close security gaps.
The stakes are high: in 2023 alone, 725 HIPAA breaches exposed over 133 million records - averaging 364,571 records per day. Civil penalties for violations can reach up to $1.5 million per year per category. Choosing the right dispatch platform not only safeguards patient privacy but also protects your business from severe financial and reputational harm.
HIPAA Compliance Checklist for NEMT Dispatchers
Having a clear checklist can help ensure your Non-Emergency Medical Transportation (NEMT) dispatch operations align with federal HIPAA regulations. This framework can guide you in auditing your processes, identifying gaps, and avoiding costly violations.
Training and Documentation Requirements
Before accessing any Protected Health Information (PHI), dispatchers must complete HIPAA-specific training. This training should be refreshed annually or whenever there are updates to HIPAA rules. Generic healthcare training won’t cut it - dispatchers need training tailored to the Privacy Rule (limiting access to the minimum necessary), the Security Rule (protecting HIPAA-compliant dispatch software), breach notification protocols, phishing awareness, workstation security, and proper disposal of devices containing PHI. Active learning methods, like quizzes or phishing simulations, are more effective than passive approaches.
Keep detailed records of all training activities, including rosters, completion certificates, quiz results, and versioned training materials. Additionally, maintain documentation such as policies, workforce acknowledgments, sanction records, risk analysis reports, audit logs, encryption standards, access control lists, executed Business Associate Agreements (BAAs), and breach logs for at least six years.
"A regulated entity must maintain documentation... until six years after the later of: 1) the date of the document's creation or 2) the date the document was last in effect."
Once training and documentation are solid, focus on safeguarding PHI across all forms of communication.
PHI Handling and Security Standards
HIPAA requires strict protection of verbal, written, and digital PHI. For verbal communication, ensure dispatchers work in private spaces where patient details cannot be overheard. Share only the necessary PHI - like pickup locations and mobility needs - rather than providing full medical histories.
Physical security measures are equally critical. Control access to the dispatch center, position workstations to prevent unauthorized viewing, enforce automatic device locks, and securely dispose of paper records by shredding them. For digital PHI, assign unique user IDs to each dispatcher, enable automatic logouts after inactivity, encrypt all transmitted data, and maintain audit logs to track access. Regularly review these logs to detect any suspicious activity.
With PHI handling under control, the next step is ensuring compliance from your vendors and technology partners.
Vendor and Technology Compliance
Your compliance efforts should extend to all technology partners and vendors. Ensure every vendor signs a current BAA, whether they provide dispatch software, cloud storage, or IT support. Store these agreements in a centralized location for easy access during audits, and confirm that vendors require their subcontractors to follow HIPAA rules as well.
When assessing technology solutions, look for features like encryption (for both data at rest and in transit), unique user IDs, automatic logouts, and detailed audit logs. Ask vendors about their incident response plans and data backup protocols. Verify that they’ve demonstrated recognized security practices within the past year. Under the HITECH Act, vendors can face direct civil and criminal penalties for HIPAA violations, making it essential to choose partners who prioritize compliance.
Conclusion: Reducing Risk Through Consistent Compliance
HIPAA compliance isn't a one-and-done task - it's an ongoing responsibility. Taking proactive steps like providing dispatcher-specific training, using HIPAA-compliant technology, and implementing clear, documented processes can help avoid costly penalties and ensure your organization stays on track.
Annual refresher courses should be tailored to real-life dispatch scenarios, making the training practical and relatable. Pair this with HIPAA-compliant software that includes features like end-to-end encryption, role-based access controls, and immutable audit trails. These tools not only help prevent violations but also strengthen your overall compliance framework.
The impact of such measures can be dramatic. Take Metro Medical Transport, for example. By embracing technology-driven compliance, they slashed their claim denial rate from 23% to 6%, boosted monthly revenue by $200,000, and achieved a spotless record during state audits.
"The average HIPAA violation fine is $1.5 million, but the damage to reputation can be far worse." – Healthcare Compliance Institute
Don't overlook the importance of extending compliance efforts to your vendors. Ensure that all software providers sign Business Associate Agreements, conduct quarterly internal audits, and appoint a HIPAA Security Officer to oversee risk assessments. Under the HITECH Act, the Department of Health and Human Services (HHS) considers whether your organization has upheld "recognized security practices" over the past 12 months when determining penalties. Consistent documentation and adherence to these practices could make all the difference.
FAQs
What can NEMT dispatchers do to stay HIPAA compliant and avoid unintentional violations?
To ensure compliance with HIPAA and minimize the risk of accidental violations, NEMT dispatchers should prioritize safeguarding sensitive patient information through a mix of clear policies, secure technology, and regular staff training.
Here are some essential steps to follow:
- Provide regular training: Make sure all staff members are well-versed in HIPAA regulations and know how to handle protected health information (PHI) appropriately.
- Use secure communication methods: Avoid transmitting sensitive details through unsecured channels. Opt for tools designed to protect PHI.
- Implement technical safeguards: Features like encryption, unique user credentials, and audit logs help monitor and control access to sensitive data.
- Enhance physical security: Limit access to devices, files, or areas where PHI is stored to prevent unauthorized use.
- Conduct regular risk assessments: Identify any weaknesses in your system and address them proactively to stay ahead of potential issues.
By combining these practices - strong internal policies, advanced security measures, and ongoing education - dispatchers can significantly lower risks and ensure they remain HIPAA-compliant.
Why is it risky to use unsecured devices for NEMT dispatch tasks?
Using unsecured devices for dispatch tasks can seriously compromise sensitive patient information. Personal devices like smartphones, tablets, or laptops without proper security measures - such as encryption, password protection, or secure access controls - can leave electronic Protected Health Information (ePHI) vulnerable to unauthorized access, data breaches, or even theft. This includes critical details like patient names, medical histories, and appointment schedules.
The HIPAA Security Rule requires organizations to implement safeguards to protect ePHI, including encryption and secure access protocols. Unsecured devices fall short of these requirements, significantly increasing the risk of violations. Such breaches don’t just lead to potential fines and legal actions - they can also harm your organization’s reputation. To maintain compliance and protect patient data, ensure all devices used for dispatch are encrypted, secure, and have remote wipe capabilities in case of loss or theft.
Why do NEMT dispatchers need a Business Associate Agreement (BAA) for handling patient information?
A Business Associate Agreement (BAA) plays a crucial role for NEMT dispatchers handling Protected Health Information (PHI). This agreement legally defines their responsibilities under HIPAA to ensure the privacy and security of sensitive patient data.
The BAA specifies key safeguards, including encryption, access controls, and secure data handling practices, aligning operations with federal regulations. By detailing these requirements, it not only helps dispatchers maintain compliance but also minimizes the risk of penalties tied to HIPAA violations. Beyond legal protection, a signed BAA reflects a strong commitment to patient confidentiality, fostering trust with both healthcare providers and patients.